Even before it opened in Presque Isle in March, the Aroostook Memory Center had 68 referrals.
Primary care physicians across the rural county had patients they suspected were experiencing some form of cognitive decline and were seeking additional support from dementia specialists. Since launching, the program has received seven or eight new patients a week.
Vi Belanger, manager of the Memory Center, which is housed within the Aroostook Agency on Aging, said the pent-up demand for dementia services speaks to the level of need in Aroostook County.
Alzheimer’s disease was among the top five leading causes of death in 2022 and the closest dementia specialist is more than 150 miles away in Bangor.
“There truly is a huge need here,” Belanger said. “We have limited primary care, and we have limited dementia specialty.”
In the oldest state in the country, a tenth of Mainers over the age of 65 have dementia — but the number of dementia specialists, across multiple disciplines, has remained low and in some cases is shrinking.
The Alzheimer’s Association has classified Maine as a “neurology dementia desert,” estimating there will be fewer than 10 neurologists per 10,000 people with dementia by 2025.
Maine had 36 geriatricians in 2021, according to the nonprofit organization, and will need to increase those ranks by about 97 percent to meet the need in 2050. Meanwhile, the number of psychiatrists in the state has been falling, with 60 employed in 2023, according to the U.S. Bureau of Labor Statistics.
Even within those fields, there are only a handful of specialists in Maine who are dedicated to studying and addressing Alzheimer’s disease and related dementias, according to several experts in neurology, geriatrics and psychiatry who spoke to The Maine Monitor.
Dr. Heidi Wierman, division director for geriatrics at MaineHealth Maine Medical Center, said it’s challenging to recruit students into geriatrics, both nationally and in Maine. Geriatric fellowships at MaineGeneral and Maine Medical Center struggle to fill their positions, she said.
“Older adults are a very complicated population, and I think for young clinicians (who are) training, it’s hard because they don’t match the textbooks,” Wierman said. “You have to not just include the medical thinking but also the environment and social influences. It can just feel very complicated.”
Geriatrics also requires another year of training in addition to three years of residency and often earns less than other disciplines. “As we joke in geriatrics, you do one more year of training to get paid less,” Wierman said.
It’s proven difficult to recruit students to Maine for a one-year fellowship, she said. Three years ago Maine Medical Center started a combined internal medicine and geriatrics residency and fellowship, which guaranteed the resident would stay a fourth year for the geriatrics fellowship.
Wierman said she’s found more success with that approach because it’s easier to get someone to come to Maine for four years and the program attracts students who are interested in geriatrics from the beginning.
While it’s important to increase the ranks of specialists, Wierman said it’s also necessary to expand the dementia knowledge of primary care physicians. In the absence of enough specialists, the pressure to diagnose can fall increasingly on primary care doctors, who are already overloaded and operating within short visits.
MaineHealth offers a program called Project ECHO, through which physicians can learn from specialists and join a network that shares expertise across the state. Wierman said an upcoming session will focus entirely on dementia, in part to bridge the gap in access to specialists.
The Aroostook Memory Center, funded by a three-year $1 million grant, serves a similar purpose. Patients are referred to the program via primary care physicians, and then interviewed by center staff. Their information is then shared with Dr. Cliff Singer, chief of the Center for Geriatric Cognitive and Mental Health at Northern Light Acadia Hospital.
Singer typically reviews between three and eight cases a week, meeting with the Memory Center through videoconferencing technology, and often selects one to be a patient at the Mood and Memory Clinic in Bangor. In the other cases, Singer provides primary care doctors with recommendations, such as conducting MRIs, ordering lab work or prescribing a certain medication.
Singer said that while telehealth visits are an inadequate replacement for patients who need specialist care, this approach identifies those who really need to travel to the clinic in Bangor and for the others, at least gets them “started down the right path.”
Belanger said she has seen clients benefit from this program. She recalled a woman in her late 70s from Central Aroostook who had noticed her memory was faltering but was embarrassed to tell her family.
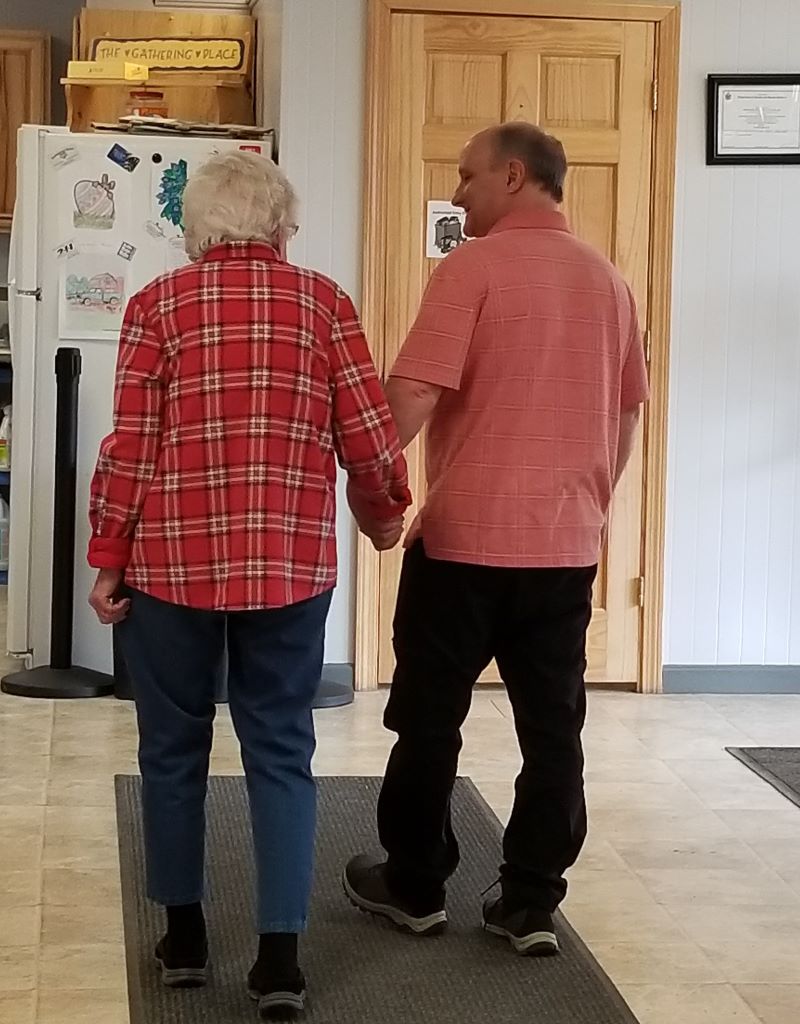
After the woman had several conversations with the Memory Center, Singer took her on as a patient and she was able to tell her husband of 58 years that she was struggling. She worried he would think less of her, Belanger said, but instead her husband took her hand and said he would be there to support her.
“She just started to cry and she said, ‘Does this mean that I have people that understand me and I’m not so alone?’ ” Belanger said.
The woman is now one of about 1,000 patients at the Bangor Mood and Memory Clinic. Singer said the clinic takes on about eight new patients a week, but it’s difficult to keep up with referrals. At one point the waitlist was two years long. It’s now about six months.
Singer said part of the challenge is that Maine lacks a strong network to connect dementia specialists with each other and with patients.
This is the first thing Dr. Justin Otis, a neuropsychiatrist at Northern Light Health and Singer’s colleague, noticed when he moved to Maine from Wisconsin a year and a half ago.
Wisconsin had a robust dementia clinic network staffed by different types of dementia specialists, where providers took a collaborative approach to getting patients to different or higher levels of care, he said. In Maine, he said, the system is more fragmented.
“The deficit is made worse by poor connectedness between providers,” Otis said. “There’s more parallel care, or duplicative care, where somebody might end up in my clinic who really should have seen a different neurology provider.”
This month, with the help of a $1.33 million one-year federal grant, Northern Light Acadia Hospital embarked on a three-pronged approach to expanding the dementia network in rural areas by improving the capacity of primary care physicians to assess, diagnose and create care plans for dementia patients; training more dementia specialists; and creating a statewide consortium of dementia specialists to help people get diagnostic assessments and get directed to appropriate treatment.
Drew Wyman, executive director of the Maine chapter of the Alzheimer’s Association, said the research around Alzheimer’s disease and other dementias is evolving rapidly, and noted that as this happens it will be increasingly important for the state to build out its network of specialists and ensure that Mainers, particularly those in rural areas, know what’s available.
“As stuff gets developed, hopefully, there will be more equitable access and options for treatments,” Wyman said. “But it all starts with early detection and accurate diagnosis. You can’t have anything without that.”
Correction: This story has been updated to reflect the official name of the center in Presque Isle. It is the Aroostook Memory Center, not the Aroostook Memory Care Center.







