In late October, while I was parsing through complicated rate methodology changes for nursing homes, I received a note from a source alerting me to the fact that the state Department of Health and Human Services had proposed unexpected and significant updates to regulations for assisted living and residential care facilities.
As I started going through the proposal, it became clear that residential care facilities would have to dramatically increase their staffing, among other new requirements.
The changes came as a surprise to many in the industry, who thought the regulations would be limited to the licensing structure. During a three-hour public hearing in November, one provider asked, “What is the basis for these proposals?”
I noticed a lot of parallels between the state’s proposed requirements and what I had found during my 18-month investigation into the largest residential care facilities published by The Maine Monitor and ProPublica.
We found dozens of resident rights violations, including abuse and neglect incidents, more than a hundred cases where residents wandered away from their facilities and hundreds of medication and treatment violations.
The experts I spoke to said requiring higher staffing levels, better training and more nursing care would help solve these issues.
The proposed regulations are even stricter for memory care units, which would be required to have staffing ratios beyond what is required in nursing homes plus one additional employee during the day shift who is tasked just with watching residents.
During The Monitor’s investigation into these facilities, experts and advocates said current staffing and training requirements for residents in dementia units are woefully inadequate.
Residents with Alzheimer’s disease and other dementias are among the most vulnerable because they can have a tendency to wander: The Monitor and ProPublica found residents left their facilities unattended at least 115 times between 2020 and 2022.
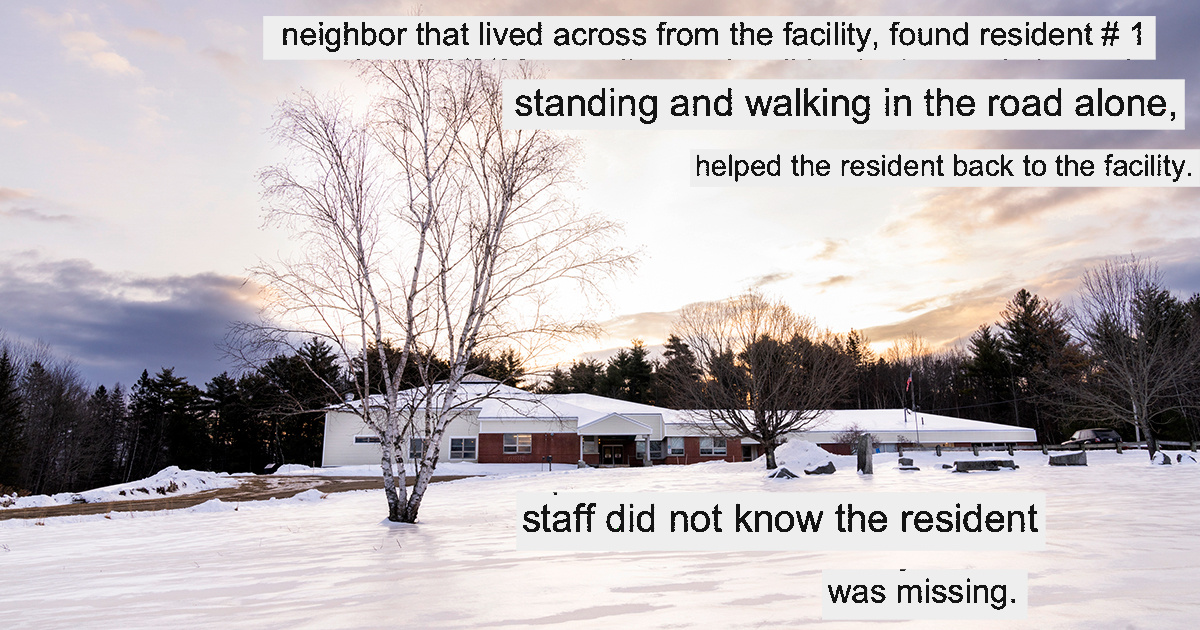
To learn more about what happened in these cases, I requested police reports and called local officials. In two cases in Cape Elizabeth and Frankfort, I learned from police reports that neighbors had found the residents and brought them back to the facility. I went to those neighborhoods and knocked on doors.
In Frankfort, I successfully reached the woman who found a disoriented resident standing in a busy street with a walker. She described to me her alarm and outrage, and provided key context for the story, including that there was only one person on staff the night of the elopement, the facility didn’t have alarms on the doors and staff didn’t know the resident had been missing.
The Department of Health and Human Services is currently going through public comment on the proposed regulations, which will then go to lawmakers.