An anonymous tip from a reader 18 months ago urging The Maine Monitor to look into two resident deaths at a long-term care home sparked our year-long investigation with ProPublica’s Local Reporting Network into Maine’s assisted living facilities.
We found that these facilities are increasingly caring for older Mainers with higher medical needs, yet face less regulation and oversight than nursing homes, even in response to serious cases of abuse and neglect.
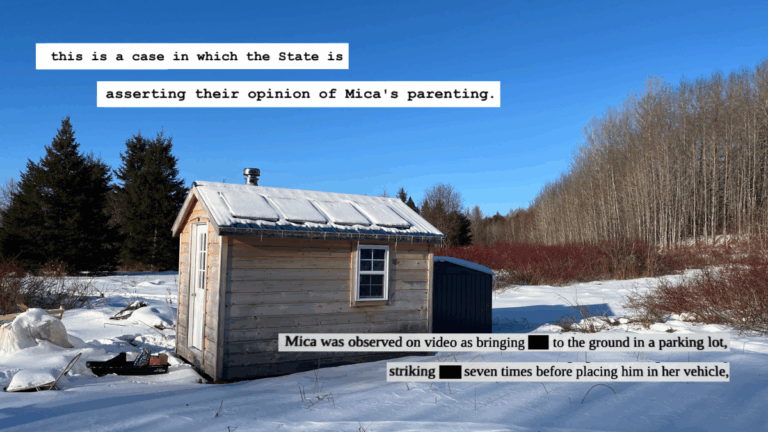
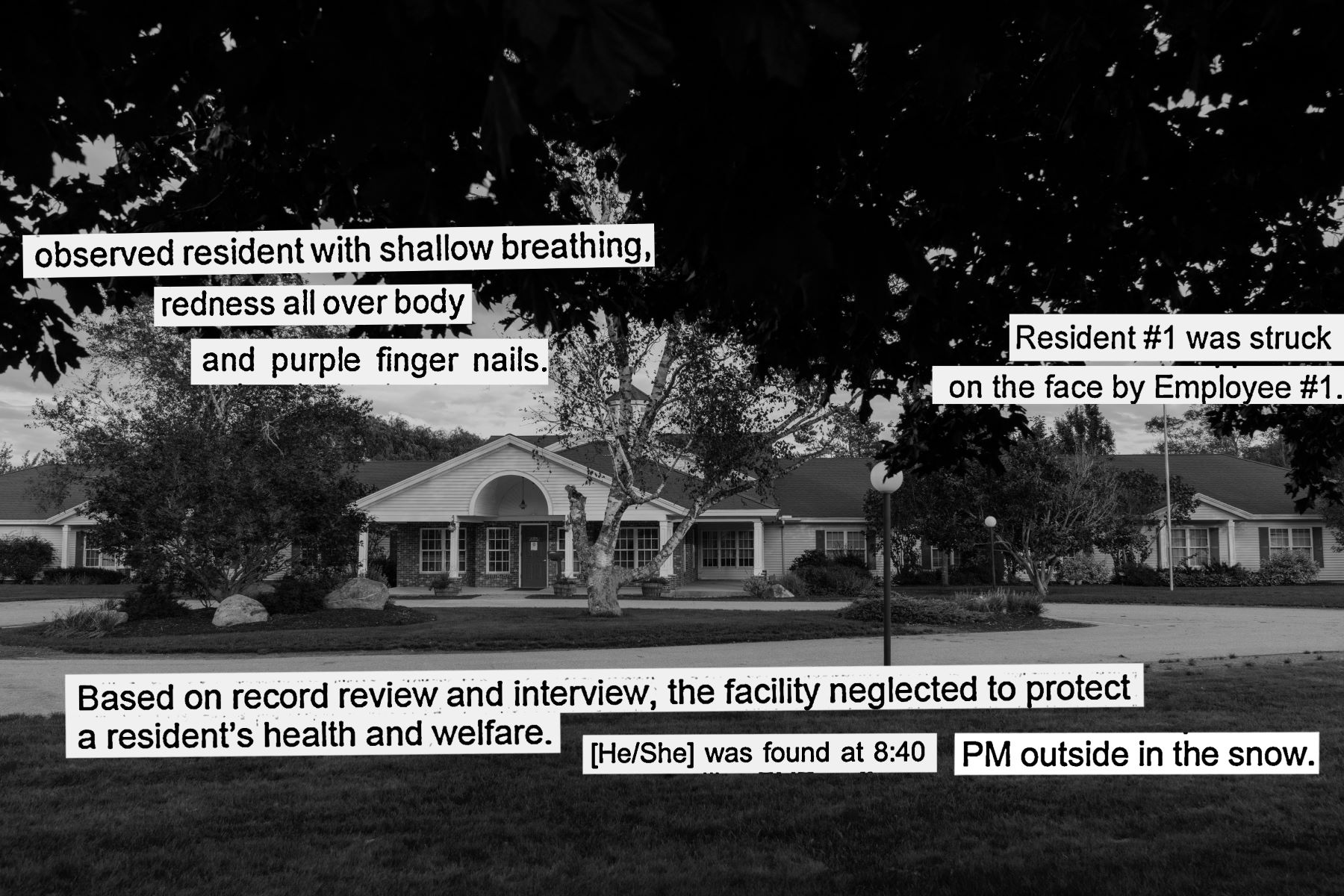
Our story broke the news that a resident at Woodlands Memory Care in Rockland died after spending two hours in an outdoor courtyard, and another resident with a severe peanut allergy had died after being served a peanut butter and jelly sandwich.
Maine’s Department of Health and Human Services investigated both incidents and cited the facility for neglect in each case; Woodlands is still appealing the findings in the courtyard case.
But the story appeared deeper than isolated incidents.
We learned that assisted living facilities are subject only to state regulations that hold them to much lower minimum staffing, nursing and physician requirements than nursing homes, which face state and federal scrutiny.
There are multiple public databases to search information on nursing homes — under the U.S. Centers for Medicare and Medicaid Services and ProPublica — but no comparable database for assisted living facilities.
There could be other cases like what we heard in the news tip, but we’d need to formally request hundreds of records from the state to find out.
So that’s what we did.
To help us undertake this project, we applied to be part of ProPublica’s Local Reporting Network, which the national nonprofit investigative news outlet established to help local reporters tackle a larger investigation. We were selected with four other newsrooms from around the U.S. and began our project in November 2022.
Since then we submitted more than a dozen formal records requests, including three year’s worth of inspection and investigation reports for all of the state’s roughly 200 Level IV residential care facilities. We chose Level IV facilities because they are the closest in size and level of care to nursing homes, but provide assisted living services and a somewhat less intensive level of care.
We received 331 inspection documents, which we parsed into more than 700 individual violations. We compiled each violation into a large database that detailed the facility, the violation type and the facility’s response on fixing the problem. Then we conducted a data analysis to find out which types of violations were most common and which facilities showed up most frequently.
The analysis showed these Level IV facilities, which the state considers “nonmedical,” were cited for roughly 200 violations involving medications and treatment.
Through interviews with nearly 100 experts, advocates, family members, providers and former employees, we learned that these facilities, which are intended to provide a lower level of medical care, are increasingly serving residents with a higher level of need.
Multiple sources said there are Mainers in residential care facilities who would have been in a nursing home 20 years ago.
To find out what has changed, we combed through reports and legislation from the mid-1990s, including a visit to the Maine State Archives. We found that lawmakers enacted a policy change tightening the medical eligibility to qualify for a nursing home in an effort to redirect older Mainers toward less institutional options while also reducing nursing home costs for the state, which were the single largest component in the state’s Medicaid budget.
State reports and data show that between 1996 and 2022, the number of nursing home beds in Maine dropped by nearly 3,680, from a high of more than 10,000. Numerous Maine nursing homes have closed in recent years. Meanwhile the number of beds in residential care facilities almost doubled, jumping by more than 4,200. As a result, older Mainers with significant medical needs live in these residential care homes.
We put a call out to readers to hear their stories about loved ones who possibly needed higher care but instead were reliant on a nonmedical residential care facility. We received more than 50 responses and are still accepting submissions.
Tania McIntyre and Melody Leavitt were among those who responded, then spent multiple Saturdays last spring telling us about their struggle accessing the right level and quality of care for their brother, Martin Hunt.

After establishing that the medical need in these facilities is higher than they originally intended to serve, we turned to the level of oversight from the state. Our database of inspection reports found that DHHS had cited facilities for 59 resident rights violations, which is a category that includes abuse, neglect and exploitation.
We also analyzed a separate dataset from the state of incidents the facilities are required to report and found that from 2020 to 2022, Level IV facilities reported more than 550 reports of abuse and neglect incidents.
Despite these violations, DHHS issued only one fine and four conditional licenses, which can include an order to stop new admissions.
In case after case, including a facility failing to report a resident repeatedly sexually abusing another resident, and another facility failing to help a resident who fell and was naked, “soaked in urine” and calling for help, the state only required facilities to submit a “plan of correction” detailing how they would address the problems.
The two incidents that sparked this investigation — the resident who died after being found in an outdoor courtyard in winter and another who died days after being fed a peanut butter and jelly sandwich despite his severe peanut allergy — both also resulted in only a plan of correction.
We are continuing to investigate Maine’s system of long-term care and would like to hear from readers. You can fill out our survey on assisted living facilities or reach out to health reporter Rose Lundy directly at gro.r1751531585otino1751531585menia1751531585meht@1751531585esor1751531585.