Falling Short: Rebuilding elderly care in rural America
Rural nursing homes across the country, already understaffed, face significant new federal staffing requirements. With on-the-ground reporting from the Institute for Nonprofit News’ Rural News Network and data analysis assistance from USA TODAY and Big Local News at Stanford University, eight newsrooms, including The Maine Monitor, explore what the rule change would look like for residents in communities across America. Support from The National Institute for Health Care Management (NIHCM) Foundation made this project possible.
Maine nursing homes are closer to meeting the Biden administration’s proposed minimum staffing standards than their counterparts in most other states, but recent payroll data show that still fewer than one in 10 are meeting these proposed standards every day.
And while some long-term care advocates said the national standards should go further, nursing home industry leaders said it would be difficult for a rural state like Maine to find the workers to meet the required minimums, which could lead to more closures.
The Biden administration in September proposed federal standards that would require nursing homes to have a registered nurse on duty at all times, and establish minimum care hours per resident from registered nurses and nurse aides.
During the second quarter of 2023 — from April to June — Maine nursing homes met the proposed minimum care hours from both registered nurses and nurse aides an average of 59 out of 91 days in the quarter, according to analysis from The Maine Monitor, USA TODAY and Big Local News at Stanford University of the latest federal staffing data. The data is collected by the Payroll-Based Journal from the U.S. Centers for Medicare and Medicaid.
Only Alaska was higher with an average of 88 days. The national average was 18 days.
However, only 8% of Maine nursing homes met both standards on all 91 days of the quarter. This still places Maine third in the country behind Alaska and Hawaii. (The national average was 1%.)
Part of the reason Maine nursing homes are more prepared to meet the standard could be because the state already has its own nursing home staffing requirements, including minimum staff ratios.
However, long-term care resident advocates and industry leaders said the biggest challenge for Maine homes would be meeting the proposed requirement for registered nurses on duty at all times.

Brenda Gallant, Maine’s long-term care ombudsman who advocates for nursing home residents and their families, praised the effort to establish national minimum standards. She viewed staffing as the most important aspect of quality of care in a nursing home. However, Gallant said, she would have liked to see the proposal go even further.
“Honestly, why is it taking the country so long to do the right thing, both by residents and staff?” she said. “We can’t expect people to want to do this work without sufficient resources and when there isn’t sufficient staffing.”
Studies have tied staffing to quality of care and called for the establishment of a federal minimum staffing standard.
The Maine Health Care Association, which represents 200 nursing homes and assisted living facilities across the state, has called the proposed minimum an unfunded mandate that could lead to more nursing home closures.
In less than three years, the number of nursing homes in Maine has dropped from 93 to 83, some of which have cited staffing challenges as part of the reason. The federal payroll data included staffing information from 85 nursing homes for the second quarter of this year, but two more have since closed.
Angela Cole Westhoff, the organization’s president & CEO, said Maine nursing homes are among the closest to meeting Biden’s proposal because the state already has some of the highest standards in the country and because Maine homes serve residents who often have higher care needs, which requires them to provide more staffing per resident.
But workforce shortages are already stressing the industry, she said, adding that there needs to be significantly more investment from policymakers to better train and pay direct care workers.
“Essentially, every single nursing home in Maine has multiple jobs posted,” Westhoff said. “We already want more staff. The issue is that Maine simply does not have the workers available to meet our needs.”
While Maine is comparatively better than most other states, the fact that other states are so low demonstrates there is a significant challenge to meeting this proposal, said Jess Maurer, executive director of the Maine Council on Aging.
The proposed rules for nurses and nurse aides would be phased in over three years for most homes, but rural areas would have five years to meet the new standards. The proposal also includes $75 million for staff recruitment and training.
Maurer said the proposal should include additional support and funding for rural communities where it will be hard to find the workers to meet these standards, especially in Maine because it is the oldest state and has among the lowest working-age population in the country.
“We’re the first in the country to deal with this, but we will not be the last,” she said. “We should be the canary in the coal mine. The Feds should be looking at how many nursing homes have closed in Maine and why and who is going to follow because they can’t meet these staffing ratios in small, rural areas.”
Best and worst performers
Even some of the nursing homes doing the best at meeting the proposed requirements were critical of the proposal.
Seven of Maine’s 85 nursing homes met both Biden requirements on all 91 days of the quarter. Among those were two Maine Veterans Homes, in Augusta and Bangor. Both locations have a five-star rating from the federal government based on staffing, health inspections and quality measures.
Rebecca Gagnon, Chief Operating Officer of Maine Veterans Homes, said the homes might have met the proposed minimum staffing requirements because they are “consistent with the unique VA regulations” they already are required to meet, such as round-the-clock presence of a registered nurse.
These existing requirements make operations more costly due to workforce scarcity, Gagnon said.
“Although Maine Veterans’ Homes assumes that the recent change proposed by CMS concerning minimum staffing requirements is prompted by a priority of ensuring care for nursing care residents, we are concerned that the mandate will have the opposite, unintended effect of complicating the availability of services for Maine’s seniors as the industry continues to struggle to meet staffing levels,” Gagnon said.
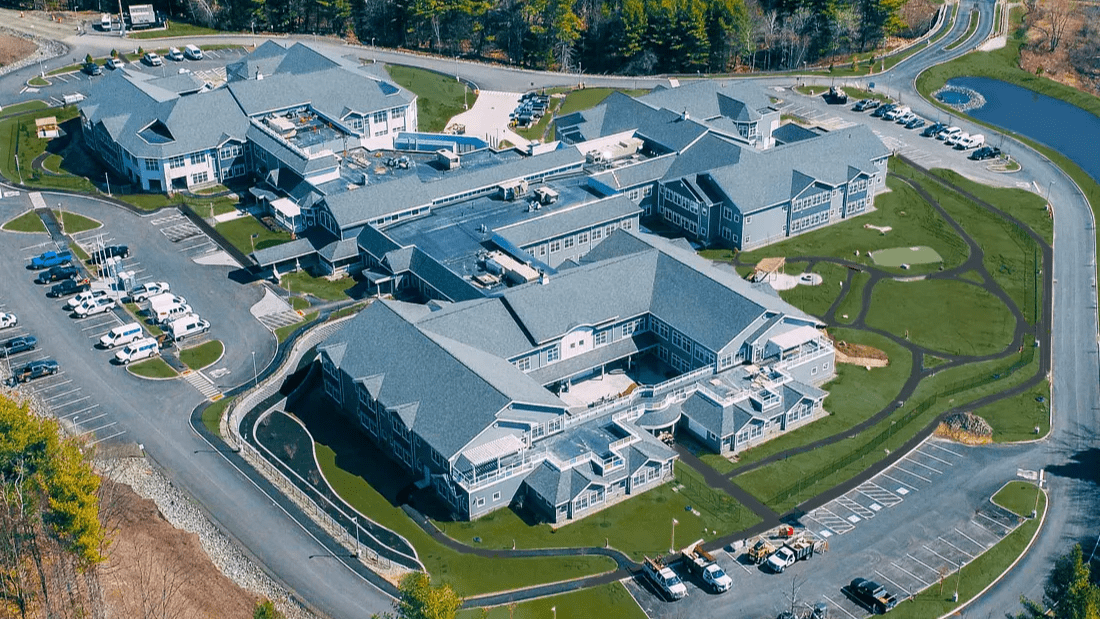
Cove’s Edge in Damariscotta also met both the proposed registered nurse and nurse aide hours on all 91 days of the quarter and has a five-star rating from the federal government. But MaineHealth, which owns and operates Cove’s Edge, said it had “serious concerns” about a national ratio.
MaineHealth is able to invest and subsidize staffing across all its facilities because it is the state’s largest health system, but it comes at a cost and stand-alone nursing homes may not be able to do the same, said Katie Fullam Harris, chief government affairs officer for MaineHealth.
The existing labor shortage, especially for nurses, is creating pressure across the entire healthcare system.
On any given day, MaineHealth hospitals have 60 to 70 people waiting to be discharged to a nursing home or rehab but there’s nothing available, she said. Cove’s Edge has an additional unit that is currently empty because reimbursements are too low to staff it, Harris said.
“If you mandate a staffing ratio for which there’s no justification, all you will do is put further pressure on a system that is already in crisis,” she said.
Four of the five nursing homes least prepared to meet the proposed standards are owned by Genesis Healthcare, which is one the largest long-term care providers in the country with nearly 250 skilled nursing homes and assisted living facilities in 22 states, according to the company’s website.
Cedar Ridge Center in Skowhegan met both of Biden’s requirements on one day of the quarter and has a two-star rating from CMS. Pine Point Center in Scarborough met both requirements on two days and has a four-star rating. Sandy River Center in Farmington met both on four days and has a one-star rating. Sedgewood Commons in Falmouth met the requirements on five days and has a three-star rating.
A representative for Genesis did not respond to requests for comment.
The proposal on the table
If Biden’s proposed minimum standards are implemented, nursing homes that accept Medicare and Medicaid would be required to provide residents with a minimum of 0.55 hours of care from a registered nurse per day and 2.45 hours of care from a nurse aide per resident per day. And a registered nurse would need to be on duty at all times.
Current standards require a registered nurse or licensed practical nurse to be on duty at all times.
Public comments on the proposal were accepted through early November.
Minimum staffing standards would improve safety and quality care in nursing homes, Xavier Becerra, secretary of the U.S. Department of Health and Human Services, said in a press release at the time.
“When facilities are understaffed, residents suffer,” Becerra said. “They might be unable to use the bathroom, shower, maintain hygiene, change clothes, get out of bed, or have someone respond to their call for assistance. Comprehensive staffing reforms can improve working conditions, leading to higher wages and better retention for this dedicated workforce.”

The Centers for Medicare and Medicaid has estimated that about three-quarters of nursing homes nationally would need to increase staffing to meet the proposal.
Maine nursing homes are already required by state law to have one direct-care staff member for every five residents during the day; one for every 10 residents in the evenings; and one for every 15 residents overnight.
These standards are very close to the three hours of care per resident from a registered nurse and nurse aides that would be required under the national standards, said Gallant, with the ombudsman program.
Gallant said she’d like to see national standards go even further and require 4.1 hours of direct care for each resident. This number comes from a 2001 study by CMS into quality of care, which recommended that registered nurses, licensed practical nurses and certified nurse aides provide a total of 4.1 hours per resident per day. (This recommendation included a standard for LPNs, but Biden’s proposal does not.)
On average, Maine nursing homes met the nurse and nurse aide minimums recommended by CMS in 2001 on 14.5 days of the quarter, according to the analysis of payroll data.
The ombudsman program has conducted focus groups with direct care workers across the state to hear about concerns. In these discussions, Gallant said she’d heard from workers who felt like they couldn’t call in sick because there was no one else to come in.
“There’s not a choice about providing sufficient staffing. Period. There’s just not. That’s what facilities exist to do: take care of people,” she said. “People want to do a good job. If you don’t have sufficient staff, it becomes impossible.”
The primary challenge in a rural state like Maine would be meeting the requirement to have a registered nurse on duty at all times, according to both Gallant and Westhoff, with the industry group representing Maine nursing homes.
“The Feds should be looking at how many nursing homes have closed in Maine and why and who is going to follow because they can’t meet these staffing ratios in small, rural areas.”
Jess Maurer, executive director, Maine Council on Aging
Nearly a quarter of Maine’s nursing homes — 20 out of 85 — met the proposed minimum registered nurse hours on every single day of the 91-day second quarter, according to the analysis of payroll data. This ratio is higher than all other New England states. Nationally, only 6% of nursing homes met this proposed minimum on every day of the quarter.
According to an analysis from the American Health Care Association, about a third — 28 out of 85 — Maine homes would currently meet a 24/7 registered nurse requirement, Westhoff said.
Low MaineCare reimbursement and workforce shortages are driving nursing home closures, Westhoff said, which causes a ripple effect across healthcare as hospitals and other facilities absorb the backlog of patients.
Rather than regulations and obligations, there should be a focus on innovation and solutions, said Maurer with the Maine Council on Aging. For example, it might be a better use of time to regulate staffing agencies, which are expensive for nursing homes and are intended as a stopgap during an unforeseen staff shortage but are increasingly becoming the norm.
And it’s long overdue to increase reimbursement rates for this work, she said.
“We should be talking about, as humans, what do we value and how do we want to receive care? And we should pay for it.”