Keri-Jon Wilson started as a hobbyist, making medical marijuana edibles on a small scale for patients suffering from chronic pain and cancer. But in 2015 she expanded her business, Portland-based Pot + Pan Manufacturing, and began to standardize her products.
“Eventually you’ve got to kind of grow up and decide if you want to grow the business, and add those additional steps and processes and best practice that comes with growth,” she said.
Despite no requirement in Maine to test medical cannabis for content or potency, Wilson has tested all of her batches since 2021.
The medical cannabis program in Maine is governed by separate regulations from the adult use, or recreational, program: While the adult use program requires testing for contaminants and potency, and includes potency limits, the medical use program requires neither.
Public health advocates and state officials want to see testing requirements aligned across both programs, but efforts to mandate testing have been met with strong pushback from the industry.
Last fall, the state’s Office of Cannabis Policy released a report pushing for required testing in the medical cannabis program, but lawmakers instead pursued broad legislation intended to reduce stigma around the cannabis industry that largely loosened restrictions in both the adult use and medical programs.
The resulting legislation, which takes effect this month, aims to make regulations around cannabis closer to those around alcohol by eliminating ID checks at the door, allowing minors to go into stores with a parent or guardian and allowing samples.
Wilson says it’s worth the additional cost to ensure the safety and quality of her product, as well as to check her processes and ensure consistency.
One time, lab results showed that an edible had five times the amount of THC it was supposed to have, 50 mg instead of 10. What could have been a large discrepancy in dose was caught before it left the building and never made it to the shelves, she said.
While she’s grateful there are strong lobbying groups on behalf of the medical cannabis industry, and she noted that many operations are transparent and safe, Wilson said it is alarming that there is such limited oversight for a medical product.
When she tells counterparts in other states that there are no testing requirements in Maine, “their jaws drop.”
“The reality is in the absence of those checks and balances, you really are just taking people’s words (for it) and that’s where it gets a little muddy,” she said.
Matt Wellington, associate director of the Maine Public Health Association, said he thinks the way to reduce stigma around cannabis use is to impose consumer protection regulations that ensure Mainers know they have accurate information about the products.
“Lawmakers have to see that the way forward for cannabis in Maine is to make sure that folks can have confidence in the products that they’re using, that the products are deemed safe, (and to) strengthen the oversight of the medical program, and make sure that we have common sense protections like testing and potency limits,” Wellington said.
Catherine Lewis, who’s on the board of the Medical Marijuana Caregivers of Maine — a nonprofit advocacy group that represents medical cannabis patients, growers and manufacturers — pushed back on the idea that caregivers are refusing to be regulated. The term “caregiver” in this context refers to those who can cultivate, manufacture and sell medical cannabis to qualifying patients, other caregivers and dispensaries.
Lewis, herself a caregiver, said she would support mandatory testing but only under certain conditions. She has concerns about the consistency and accuracy of lab testing, and worries the expense of testing could push small-batch caregivers out of business.
Lewis wants the state to set more explicit testing standards for private labs to ensure their processes are the same, and she doesn’t think the medical program should be subject to as rigorous testing as the adult use program due to the smaller size of their operations.
“The state has refused to meet us in the middle with the testing requirements so we’ve had to fight to kill it completely,” she said. “If we allow them to put the laws in place the way they have for adult use, the medical industry and smaller producers would crumble, and patients would lose access to their medicine.”
Regulatory debate
The medical cannabis program in Maine evolved before the adult use program and has separate regulations. When the medical use program was started in 1999, there were fewer businesses and they were small operations.
After Maine voters approved recreational marijuana use in 2016, there was an extensive public process to establish regulations and protections, which were adopted in 2019.
The state requires that recreational marijuana products be tested in their final form before they are sold to check for mold, toxins and other harmful chemicals. The products are also checked for THC potency and homogeneity; the potency limit for edible cannabis is 10 mg per serving.
The field of medical cannabis has no testing requirements nor potency limits.

Linda Frazier, who was involved in the regulatory process for the adult use program in 2019 as a public health consultant, said the intention was to establish a regulatory framework for the recreational program, then to update the medical use program to align with the new framework.
But the medical cannabis industry pushed back, Frazier said, voicing concern about changing the regulations too much and too fast, and worried about the financial impact on businesses.
“Right now the loudest people in the room the committee is listening to and the legislature hears from are medical providers,” Frazier said. “They’ve become very organized and their message has been very clear that to implement more restrictive marketing and testing … has a fiscal impact on them that they feel is unnecessary and unfair. They’ve been very successful with that messaging.”
Lewis, with the caregiver group, said it would not make sense to require the same level of testing for the medical cannabis program as the adult use program because the medical caregivers often are home-based programs and make small batches, so extensive testing requirements would significantly cut into their profit margin.
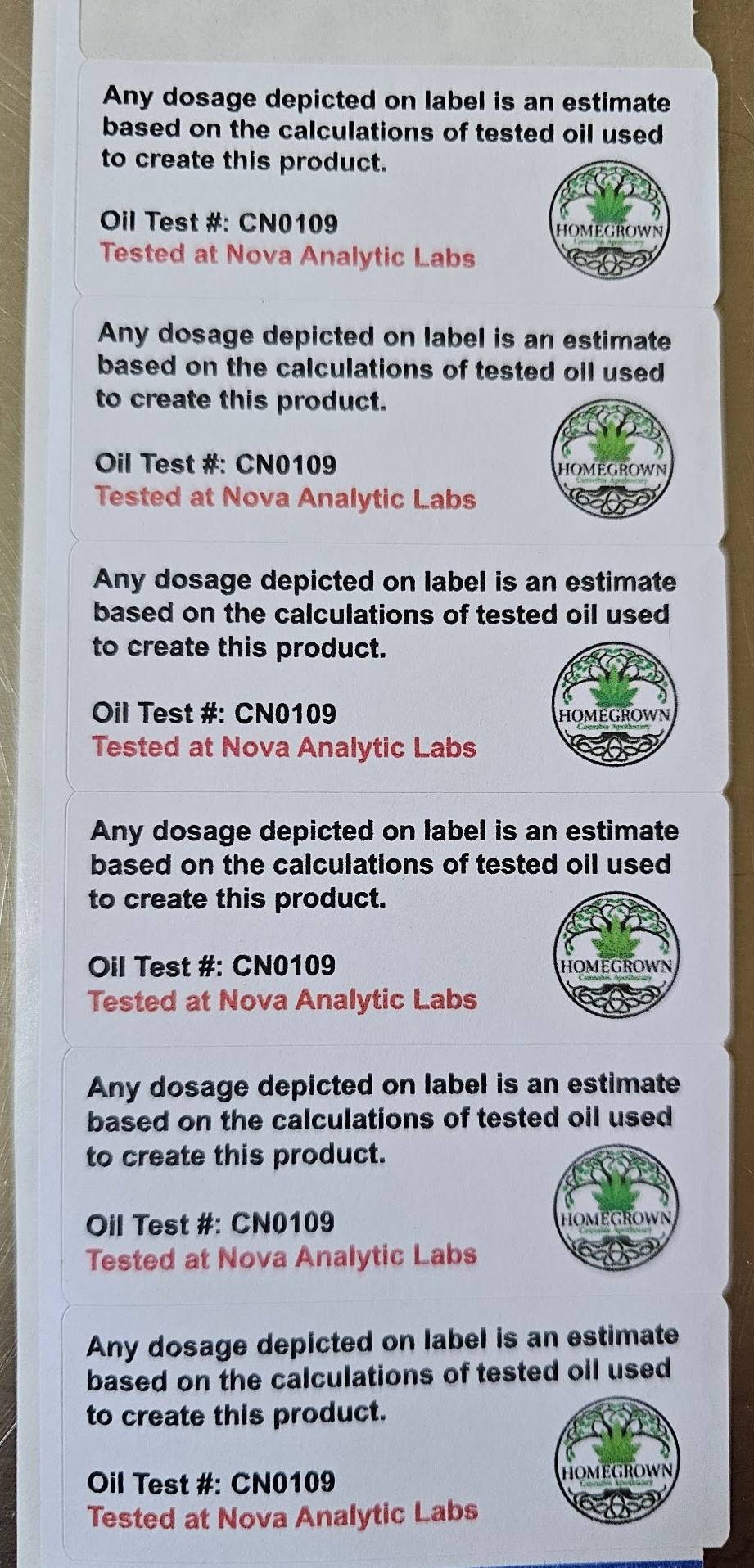
Instead, she said manufacturers should be required to test the oil before making a product, then spot-check final products and ensure the dose calculations were correct. She suggested that any product that has not been tested could be labeled “not tested.”
Testing requirements
John Hudak, director of the Office of Cannabis Policy, said one of the first things he noticed when taking over in 2022 was the medical program lacked a testing requirement, despite hearing from patients assuming there was one.
“We kept hearing from the medical cannabis industry to essentially just trust them that everything was clean. We decided to test that question and provide as much information as we could to medical patients,” Hudak said.
Last fall his office tested 120 samples from medical cannabis sellers across the state and found 42 percent had at least one contaminant that would have prohibited them from being sold on the recreational market, including pesticides, heavy metals, yeast and mold. The most common pesticide detected, myclobutanil, “releases cyanide gas upon combustion and causes a range of mild to severe effects when inhaled,” according to the report.
Lewis, with the medical cannabis industry group, said she had concerns about the sample size of the report and wondered what precipitated the test when she had heard few stories about patients getting sick from the products.
Hudak said he has not conducted a similar study on the potency of medical cannabis, but his agency has tested products on a case-by-case basis when consumers raised concerns. In a recent example, he said an edible that was supposed to be 10 mg tested at 120 mg.
Overconsumption is rarely fatal, but can include nausea, vomiting, intense fatigue and even hospitalization, Hudak said.
Testing is required for medical programs in most other states, he said, calling it the national standard. A 2022 study from Safe Access, a medical cannabis patient advocacy organization, found that of the 35 states with medical cannabis programs, Maine was one of the two without required testing. The other was Louisiana.
Hudak said he believes the opposition in Maine is a small but vocal minority that has been able to stave off previous attempts at regulations.
Rather than piecemeal changes to the medical program, Hudak said a massive overhaul is needed. The program is “wildly outdated,” he said, and a testing requirement would be a good place to start.
In response to concerns about the cost of testing, Hudak said the price of recreational marijuana has decreased despite the rollout of mandatory testing requirements. An OCP dashboard shows the average price per gram of bud/flower decreased from $15.83 to $7.30 between 2020 and 2024.
“If producing uncontaminated cannabis — that is demonstrated to be uncontaminated — is too expensive, you probably shouldn’t be producing medicine for patients,” he said.
“Absolutely,” Lewis said in response when The Monitor shared his comment. “But who is to say it’s contaminated?”
She said she’s sent portions of the same sample to different labs; it passed one lab and failed another. Without set standards from the state, she worries about the consistency of the lab results.
Hudak’s office studied this question by examining nearly 8,000 potency test results for cannabis flower at three certified labs over a two-year period and found “the variation in potency is explained by the cultivator and not the cannabis testing facility.”
Safety monitoring
Barry Chaffin, co-founder of Nova Analytic Labs in Portland, said he has many medical caregiver clients who voluntarily test their products to monitor safety and quality. In the last year, Chaffin said he has tested about 80 recreational and 190 medical accounts.
In the recreational industry, a producer must select a sample from each batch and get it tested before selling it, Chaffin said. If the batch fails, it sometimes can be remediated. For example, if cannabis flower failed for microbials, there might be a way to kill the microbes. Other contaminants, like heavy metals, can’t be remediated and the client would have to destroy any batch where they are found, Chaffin said.
There’s no potency limit for recreational cannabis flower, so if it tests at a higher potency than expected, the product would simply be labeled at the higher dose. There is a potency limit for edibles, so if those exceeded the limit, they would need to be remade or destroyed, he said.
Chaffin said there should be a regulatory framework for testing in the medical cannabis program, but like others noted that the pushback from industry groups has been strong.
“There are a lot of politics at play when it comes to any kind of regulatory framework on the medical program,” he said. “There’s some very strong feelings on having it regulated and there’s very strong feelings against having it regulated.”
Lewis said the medical and adult use industries worked well together during the past legislative session, but they don’t want to see the programs merged because they serve different populations.
“They are overregulating adult use and under-regulating medical,” she said. “It would be nice to see it meet somewhere in the middle.”
Rose Lundy can be reached at gro.r1769392559otino1769392559menia1769392559meht@1769392559esor1769392559.