A year-old law seems to have done little to curb a surge in violence against health care workers that began during the pandemic, despite increasing charges for assaults on nonmedical staff — such as custodial, security or administrative workers — who are providing emergency medical care.
According to Maine’s Judicial Branch, there have been 12 charges of “assault on an emergency medical care provider” in 2024 — on track to meet similar numbers as the last five years. There were 27 charges in 2023 and 25 in 2022, for example.
Joe Bragg, a registered nurse and nursing supervisor at Down East Community Hospital in Machias, said the expanded definition doesn’t seem to be changing the behavior of patients, many in a state of crisis when they arrive in the emergency department.
“I don’t think anybody is going into the hospital going, ‘Well, I better not act out today because L.D. 1119 is in effect,” said Bragg. “It doesn’t change anything. If violence is going to happen, it’s going to happen.”
The law – L.D. 1119 – which passed in July 2023, increased charges for an assault occurring in an emergency department setting, regardless of whether the victim is a health care worker, from a Class D crime — punishable by up to 364 days in jail and a $2,000 fine — to a Class C crime, punishable by up to five years in prison and a $5,000 fine.
(Felonies are typically crimes punishable by more than a year in prison, while misdemeanors are typically considered less serious crimes punishable by less than a year in jail. Maine no longer uses these categories.)
Between 2017 and 2021, Maine health care workers filed 1,000 claims for lost time due to intentional injury, most related to interactions with patients.
Prior to the new law, health care workers filed 167 intentional injury lost time claims in the first seven months of 2023; 114 were filed in the first four months after the law took effect.
Advocates for the expanded law, including Maine’s two largest health care conglomerates, MaineHealth and Northern Light Health, say the changes were intended to help law enforcement and prosecutors hold people accountable for their behavior and to protect those not previously included, such as security officers.
“L.D. 1119 really doesn’t impact the number of assaults, it simply clarifies the ability to prosecute,” said Jeff Austin, principal lobbyist for the Maine Hospital Association.
Austin said MHA is seeing around 200 incidents per month at its member hospitals, similar to years prior.
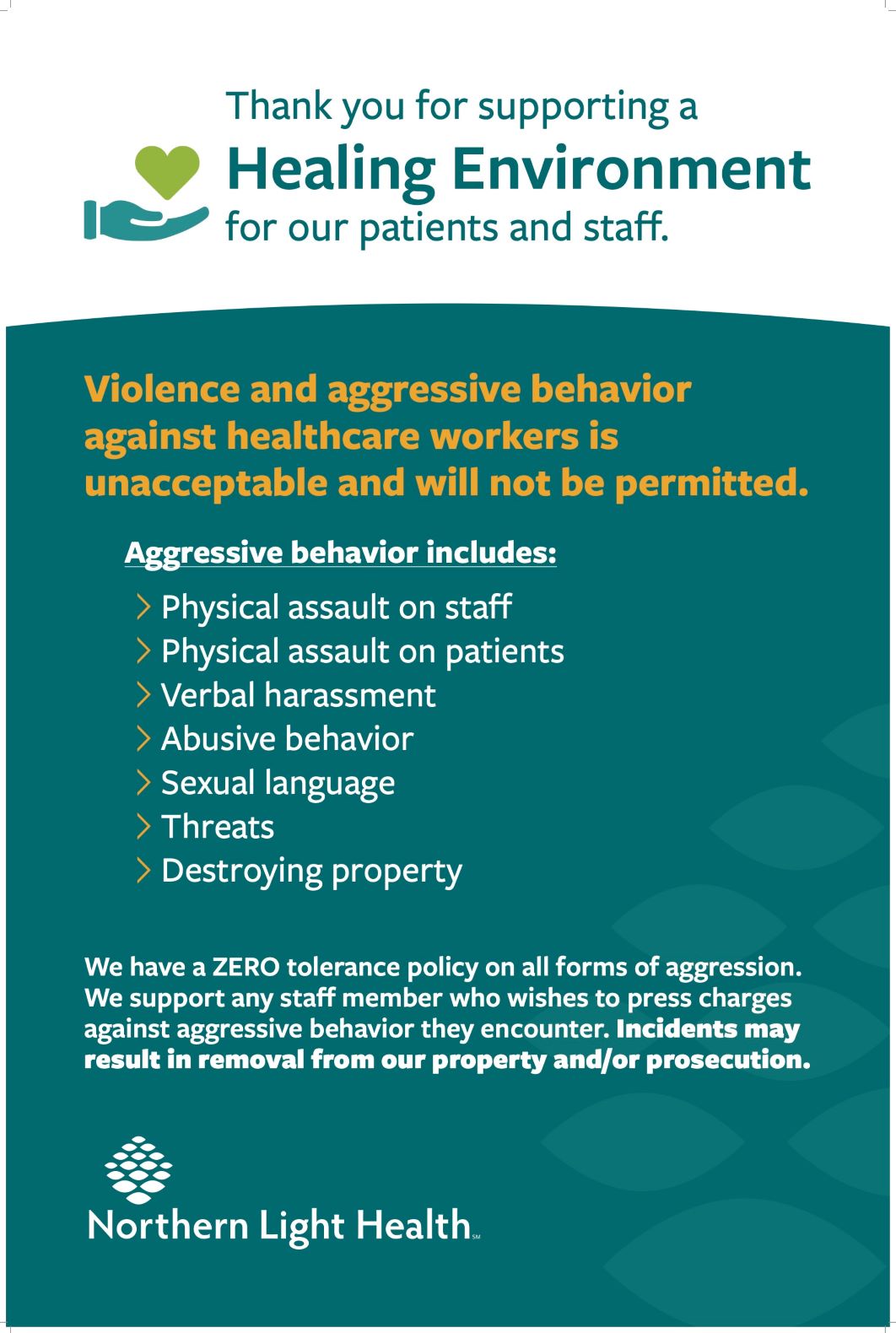
To further help combat workplace violence, hospitals have put out campaigns. The Northern Light Hospital system is working to get the ‘Safety from Violence for Healthcare Employees’ Act passed in Congress. At DECH in Machias, administrators have hung signage encouraging a safer environment and reminding visitors to “be kind to our staff.”
While violence in emergency departments predates the pandemic, its ongoing effects have added to the frequency of assaults.
In testimony last year, a registered nurse within the MaineHealth system described a patient throwing a chair at a sliding door, shattering the glass before grabbing her arm.
In another instance, Nancijean Goudey, the director of emergency services at Maine Medical Center, described a patient who lunged, grabbed her around the neck, threw her on a bed and attempted to climb on top of her.
In testimony, emergency providers described attacks that ranged from spitting to verbal abuse to physical violence. The Maine Medical Center emergency department reported 277 incidents of workplace violence in a three-month period in early 2023.
Nurses and hospital staff pushed for the passage of the law, arguing that something needed to be done to help with the violence and protect nonmedical staff.
Defense attorney Walt McKee believes classifying assault on emergency health care personnel as a felony can be a slippery slope — the person’s job should not be part of the consideration, he said.
“A felony level crime should be dealt with when there is significant bodily harm, not because it was on a nurse and not a teacher,” said McKee.
Criminalizing mental health
Others argue the expanded law hasn’t helped deter violence in the year since it was passed and that it adversely affects those with mental health issues, who may be more likely to act violently in emergency settings.
Advocates on both sides agree that violence against hospital staff should not be tolerated. But with mental health treatment resources across the state increasingly strained, those in crisis have few places to turn beyond an emergency room.
There are only 10 inpatient psychiatric treatment facilities across Maine, with roughly 500 beds. The long waitlist of people seeking mental health treatment only continues to grow, with wait periods stretching for months.
Facing a lack of resources and appropriate treatment, people turn to their hospitals, said state Rep. Nina Milliken (D-Blue Hill).
“The message is if you have a medical issue, just go to the emergency department,” said Milliken. “These systems are operating as our only response currently to a long list of human suffering. It isn’t fair to the criminal legal system, it isn’t fair to ER staff, and it isn’t fair to anyone else.”
The new law punishes people — some of whom may be in a state of psychosis and unaware of their actions — “for something that is essentially a treatment failure,” said Emily Mott, staff attorney for Disability Rights Maine.
People in crisis brought to an emergency department against their will because they are deemed a danger to themselves or others are often more at risk of lashing out, although they may not be fully in control — or even aware of — their actions.
That was the case for Julie Potter, who brought herself to the emergency room for a dissociative episode while studying for her master’s in social work at the University of New England.
Potter said after explaining her situation to hospital staff that she was led by police officers to a sterile room. Potter said she tried to leave, and remembers only waking up to bruises on her body with officers saying she had assaulted them.
Potter was eventually charged with assault on a police officer — a charge that carries similar punishments to those under L.D. 1119.

While the charges were eventually dropped, after what she said was a lengthy court proceeding and a year of psychiatric supervision, the incident upended her life and ultimately resulted in Potter leaving her master’s program.
“What it’s going to do is criminalize people’s trauma in mental health,” Potter said of the expanded law. “We are going to have more people in prison, in jails, in the court system that are just hurting and more hopeless, and do not believe in a system that cares about them. … You are ruining people’s lives.”
People convicted of felony may have trouble getting jobs or housing, said Mott, of Disability Rights Maine, which can further delay treatment.
“In a world of collateral damages, it’s important.”
Health care workers shouldn’t have to tolerate assault, said Frayla Tarpinian, district defender at the new Capital Region Defender’s Office, but expanding the law will not effectively deter violence if the behavior is driven by mental illness and the punishment doesn’t include treatment.
“There is just something manifestly unfair about somebody who does not want to be touched to be forcibly medicated, then charging them because they don’t comply.”
Who benefits?
“It’s a tough situation all around. Who does it help the most? The irony is, it probably helps prosecutors, judges and defense attorneys,” said Brendan Trainor, district attorney for Penobscot County. “It does give us more options to charge somebody.”
Despite this, many district attorney offices and police departments across the state say they have not seen an increase in the number of charges since the law was passed.
Portland Police Department, which services one of the largest hospitals in the state, Maine Medical Center, has only seen four charges since the law was enacted, despite the hospital reporting large numbers of assaults.

Other departments, including in Augusta, Lewiston and Machias, said they had seen little change in the number of charges since the law’s passage.
In Penobscot County, there have been eight charges for assault on emergency medical service personnel since July 2022. The Lewiston Police Department reported six charges between July 2023, when the law was enacted, and this June, and the Augusta Police Department reported four — on par with the 10 and seven charges, respectively, reported in the year prior.
On the other side, McKee, the defense attorney, felt prosecutors already had enough “tools in the toolbox” to charge someone with assault. Unless judges said they were seeing serious offenses that require more serious charges, he said, there was no reason to increase the penalty.
Health care providers emphasized they do not file charges against a person in a mental health crisis, unable to distinguish right from wrong. Once charges are brought, whether a person is competent to stand trial is decided by the state’s forensic evaluators and a judge.
Austin, of the Maine Hospital Association, and hospital staff recognize that violence can be unintentional, especially if it stems from someone with a mental illness.
But that’s not true for all, said Austin.
“And we believe [they] should be held accountable for their decisions.”
Alexa Foust can be reached at gro.r1751427658otino1751427658menia1751427658meht@1751427658axela1751427658.