As Maine’s COVID-19 cases continue to surge, the state’s top coronavirus official asked Mainers on Friday to change their mindset about the coronavirus in order to “change the trajectory” of the outbreaks.
In the past week, from Nov. 14-20, the Maine Center for Disease Control and Prevention opened 40 investigations into new outbreaks. Director Nirav Shah said there’s a direct link between community spread, household gatherings and eventual outbreaks.
“Earlier in the pandemic, what was for so many of us an abstract concept is now very real,” Shah said on Friday. “We need today, as a state, to update our understanding so that we can update our behavior. If we don’t do something different, nothing is going to change. We will stay on this trajectory of increasing cases, (and) each passing day will make it harder and harder to put a lid on things.”
There are a number of ways the pandemic is “fundamentally” different than it was this spring, Shah said.
Transmission this spring was related to “focal” outbreaks, often in places like long-term care facilities. Now, the outbreaks are driven by community transmission. New cases initially arose in urban areas, in populous states, after large gatherings and among older populations, Shah said. Now, outbreaks are occurring from smaller gatherings, in less-populated states, in rural areas and among younger people.
“What we’ve been seeing for weeks now is that the ground has been seeded with ever-increasing numbers of COVID-19 cases and we’re now starting to see patches in the form of outbreaks emerge all across the state,” Shah said. “Sadly that trend is one that may continue.”
Four public health experts told The Maine Monitor in August that the metrics they use to track a state’s COVID-19 response include the percentage of positive COVID-19 tests, the number of new cases, the volume of testing, hospitalization rates and the level of adherence to safety precautions.
RELATED: Navigating number fatigue: How to understand COVID-19 in Maine
Based on all but one of these metrics, Maine is in a worse place than it was over the summer. The state has broken its record for new daily cases numerous times in recent weeks, with the latest peak of 247 new cases coming on Nov. 12. The Bangor Daily News reported that more Mainers died in the first two weeks of November than in the two previous months combined. And new hospitalizations this month reached the highest peak since early summer.
Maine also has significantly ramped up testing. In early August, the volume of tests was about 171 per 100,000 people. The volume now stands at 646 tests per 100,000 people.
The state’s seven-day positivity rate — the measurement of how much a state is testing and whether its number of confirmed cases is reliable — was still only 2.9 percent on Nov. 20, Shah said. While that’s higher than rates Maine recorded this summer, it’s still below the 5 percent level recommended by the World Health Organization. Other national tracking tools, including the COVID Tracking Project, COVID Act Now and Johns Hopkins University’s Coronavirus Resource Center, record positivity rates differently and found an even lower seven-day positivity rate in Maine on Nov. 20, at 2 percent. As of Friday, only six other states have a rate below 5 percent, according to Johns Hopkins University.
Shah said the recent surge in cases is coming from within Maine and that there is no evidence that the outbreaks are from outsiders entering the state. Rather, the rising number of cases is tied to colder weather driving people to gather indoors, where they are exposed to others before going back out into the community.
He added that it’s important to pay attention to what numbers can’t capture: “The anguish, the concern and the fear that comes with having a friend or family member be hospitalized or on a ventilator with (COVID-19), as well as the mental toll that health care providers suffer from having to care for COVID-19 patients day in and day out.”
“In short, not everything that matters can be measured when it comes to COVID-19,” he said.
In related news, a Nov. 13 report from the U.S. CDC concerning an outbreak linked to an August wedding in Millinocket found that the event exceeded Maine’s 50-person limit for indoor gathering in a shared space and that wedding guests did not comply with mask requirements.
The wedding “was the likely source” of outbreaks at a long-term care facility and a correctional facility, and led to 177 cases, seven hospitalizations and seven deaths, the report found, “highlighting the importance of adhering to recommended mitigation measures even in communities where transmission rates are low.”
Robust contact tracing linked these “seemingly disparate outbreaks,” according to the report.
Current outbreaks in Maine
The Maine Center for Disease Control and Prevention has opened 40 investigations into new outbreaks across the state since Nov. 14.
“This is a long list and it’s indicative of where we are with respect to COVID-19 across the state,” Maine CDC Director Nirav Shah said Friday.
Here are the outbreaks reported over the past eight days:
- Becket House at Belgrade: Four cases
- Calais Elementary School: Four cases
- Caravel Middle School in Carmel: Three cases
- Church of Faith in Skowhegan: Three cases
- Eric Knowlton School in Berwick: Three cases
- Hibbard Nursing Home in Dover-Foxcroft: Three cases
- Lewiston Middle School: Three cases
- Maine Department of Transportation Western Region Facility in Wilton: Five cases
- Pinnacle Health Care in Camden: Five cases
- Rockland Marine Corporation: Six cases
- York High School: Four cases
- Bath Iron Works: 10 cases
- Dielectric in Raymond: Four cases
- Good to Grow Childcare in Eliot: Three cases
- Southern Maine Health Care Goodall Hospital Mental Health Unit construction site in Sanford: Four cases
- Greene Central School: Four cases
- Marshwood High School in South Berwick: Three cases
- Upper Kennebec Valley High School in Bingham: Eight cases
- Volunteers of America facility: Three cases
- Windham High School: Three cases
- BMW in Westbrook: Four cases
- Bowdoin College: Three cases among students and one among staff
- Mooring on Foreside in Cumberland Foreside: Two residents and one staff
- Berlin City Auto: Three cases
- Huntington Common in Kennebunk: Four residents and four staff
- Paris Elementary School: Three students
- Cove’s Edge in Damariscotta: Four staff
- Maine Medical Center in Portland: Four cases
- Whitefield Elementary School: One student and three staff
- Tabernacle of the Congregation in Bridgton: Three cases
- Worcester Wreath Company: Three cases
- Augusta Calumet Social Club: Three cases
- Clover Health Care in Auburn: Three staff
- Downeast Transportation: Three cases
- Edward Little High School in Auburn: Two students and one staff
- Farrington Elementary School in Augusta: Four cases
- Lewiston High School: One student and two staff
- Little Hands Childcare Facility: One child and six staff
- North East Mobile Health Services in Rockport: Four staff
- Otis Elevator Company: Four staff
Unprepared for the COVID-19 pandemic
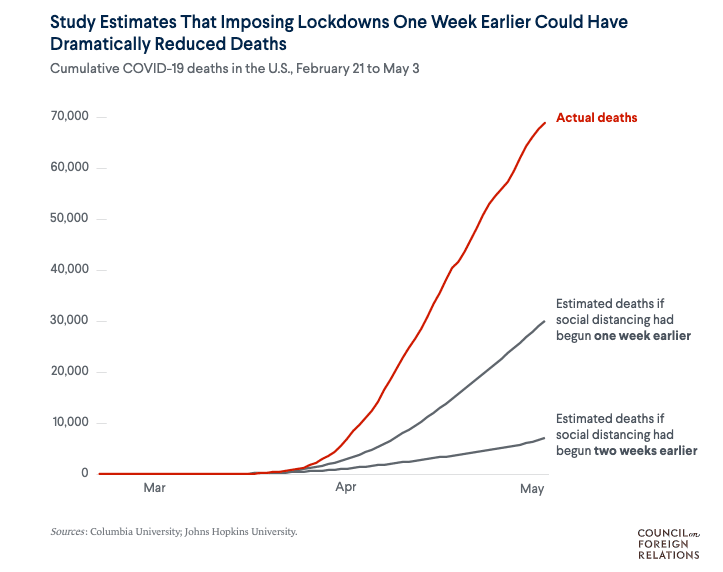
The U.S. response to the coronavirus pandemic was “deeply flawed” and significant investment is required to prepare for pandemic threats in the future, according to an independent task force report published last month by the Council on Foreign Relations.
Pandemics are inevitable but the U.S. and world should have been better prepared, according to the report. Global preparation efforts “provided the illusion — but not the reality — of preparedness.”
“Despite a succession of previous global public health emergencies, the United States and other governments failed to invest adequately in prevention, detection and response capabilities to protect the populations most vulnerable to infectious disease outbreaks, or to fulfill their multilateral obligations to international organizations and to one another,” the report continued.
The task force is co-chaired by Sylvia Mathews Burwell, former secretary of health and human services under President Barack Obama, and Frances Fragos Townsend, former chair of the White House Homeland Security Council under President George W. Bush. There are 22 public health and international policy experts on the panel.
The U.S. government did not act fast enough and wasted weeks that could have been used to create a national strategy, and ramp up testing and contact tracing, according to the report.
“These failures had grievous economic and health consequences, forcing states, localities and employers to resort to blunt interventions, including imposing severe limits on human movement, and shuttering businesses and public places,” according to the report. “Without clear federal guidance, many states relaxed these public health measures prematurely, resulting in new spikes.”
U.S. elected officials, including President Trump, failed to offer “science-based” information about the threat of infection or defend public health officials, the report found. And the nation’s underfunded state and local health systems “were quickly overwhelmed.”
“More generally, COVID-19 revealed tremendous confusion over the respective responsibilities of federal, state, local and tribal governments, resulting in blame-shifting and an incoherent U.S. approach to this public health emergency,” according to the report.
In addition, there was a lack of global coordination. China’s reporting and information sharing in the early days of the outbreak was “at best flawed,” and the World Health Organization “prioritized solidarity in its international crisis response, proving hesitant to criticize China publicly over these flaws.”
“The COVID-19 experience confirms that WHO has an important leadership role in the health aspects of public health emergencies but lacks the geopolitical heft to address the broader diplomatic, economic and security implications of pandemics,” according to the report. “The U.S. decision to pull out of WHO, if it occurs as scheduled in July 2021, threatens to make the agency’s leadership role even more precarious and the United States even more vulnerable to future pandemics.”
President-elect Joe Biden has promised to reverse the decision to pull out of WHO.
The report recommended:
- Treat pandemic preparedness as a serious national and global security threat — and invest accordingly: Designate a senior White House official to focus on public health; adequately fund WHO’s Health Emergencies Program; and establish a permanent global health security coordinator with the United Nations.
- Adopt strategies for better prevention: Establish preparedness capacity assessments; generate community mitigation guidelines and pandemic response triggers; and invest adequately in public health and provide protections to marginalized, at-risk and underserved groups.
- Improve detection of epidemic threats: Hold a review conference to discuss compliance, increase information sharing and transparency, and enhance the competence and consistency; and build a global epidemic surveillance system.
- Strengthen U.S. and global pandemic response: Develop and fund national testing and contact-tracing strategies that can be scaled up in an emergency; ensure resources for the Strategic National Stockpile; and support mechanisms to develop and deliver COVID-19 vaccines “in a globally fair manner consistent with public health needs.”
“The only certain thing is that when this pandemic is brought under control, another will eventually take its place,” according to the report. “Pandemic threats are inevitable, but the systemic U.S. and global policy failures that have accompanied the spread of this coronavirus were not.”
Public education, higher ed employment losses
Employment at Maine public colleges and universities has dropped more than 20 percent — a change of 2,600 jobs — compared to last year, according to the Pew Charitable Trusts. Only four states experienced a larger decline.
Nationally, higher education employment fell 10.6 percent in September compared to a year ago, according to non-seasonally adjusted estimates from the Bureau of Labor Statistics cited by Pew. The nonprofit tied many of the furloughs and layoffs to delayed school reopenings and canceled classes due to the COVID-19 pandemic.
When compared to the start of the pandemic in February, employment in higher education nationwide was down 13.7 percent in October.
Employment in public education (K-12) jobs in Maine has dropped 11.5 percent since last September — a loss of 4,300 jobs. Nationally, local education was down 6.9 percent during the same period.
“Although teachers account for a portion of the local education cuts, anecdotal evidence suggests that bus drivers, food service personnel, support staff and other non-instructional positions bore the brunt of the initial reductions as schools shifted to distance learning,” according to Pew.
Nationwide, state and local education employment, coupled together, declined nearly 9 percent in October compared to 2019, “representing the lowest national jobs total at that point in the school year since 2000.”
Many of those job losses may be temporary. An estimated 70 percent of unemployed state and local government workers reported their layoff was temporary in the federal government’s September Current Population Survey, according to Pew.
“The severity of public employment declines so far varies considerably across states, which isn’t surprising given that some state and local budgets have been hit harder by the new recession than others, and that schools have taken different approaches to reopening with in-person or remote instruction,” according to Pew.
In some good news, Maine CDC Director Shah said this week that while COVID-19 cases have been detected in schools, there have been few instances where the virus has spread within the school.
“That’s an encouraging finding and a clear sign that many of the difficult steps that educators, school officials, and parents and students themselves have been taking are working,” he said.
Wearing masks, installing plexiglass dividers, maintaining physical distance and adjusting extracurricular activities “are having an effect,” Shah said, and demonstrate that in-person learning can be done safely.
“If we want to keep kids in school for in-person education, the best thing we can do is to keep a lid on community transmission.”