As money from national settlements with companies accused of fueling the opioid epidemic has begun flowing into Maine, a debate has emerged between advocates, local and state governments, and on-the-ground providers over spending priorities for addressing the crisis.
Earlier this month, a nationwide coalition of more than 130 public health groups, legal aid organizations and service providers, including three from Maine, issued a “roadmap” of priorities for opioid settlement spending. Among their recommendations are to expand access to medication-assisted treatment, increase housing support for people actively using drugs or are in recovery, and support for community-based organizations doing on-the-ground work.
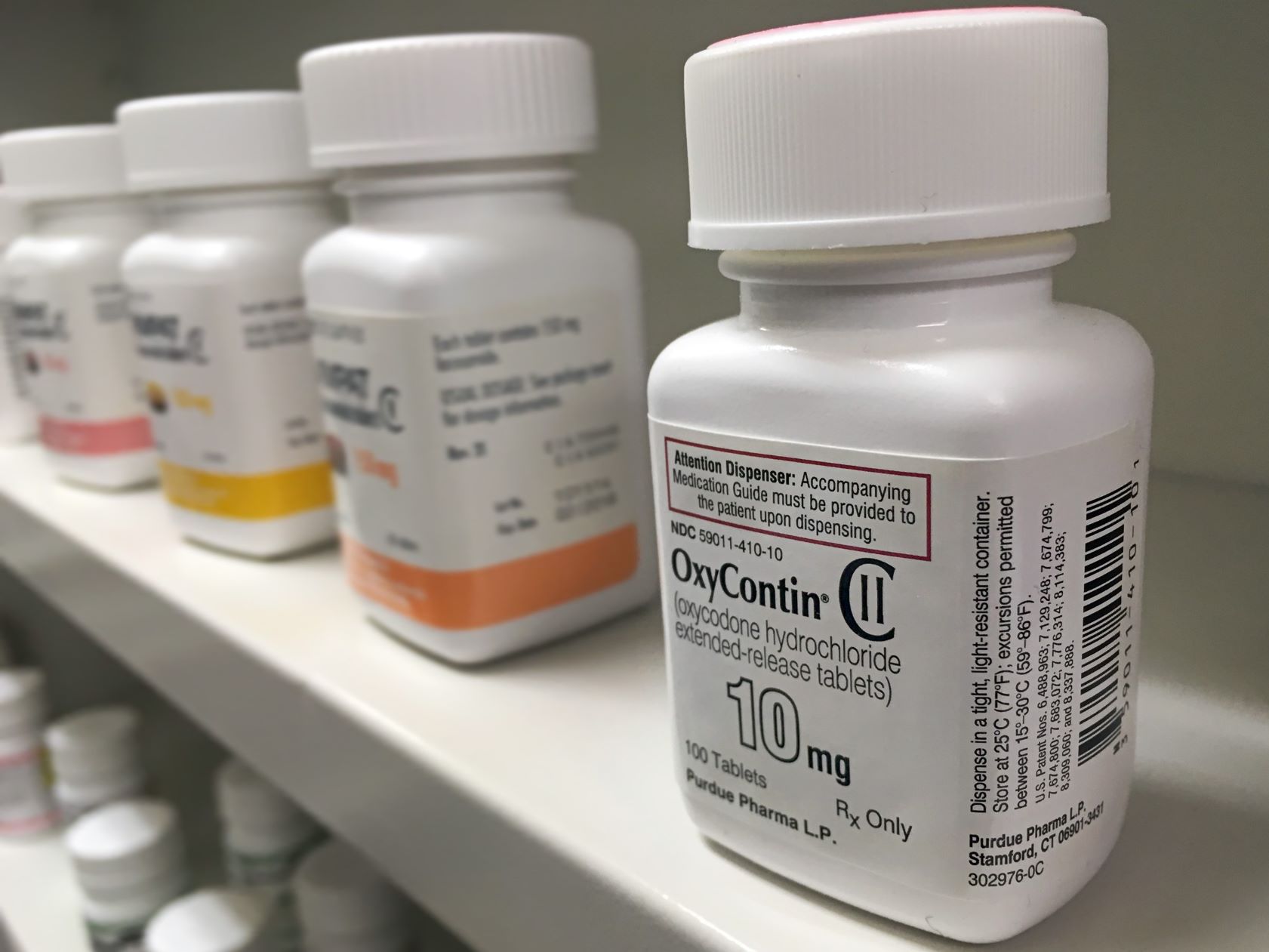
The multi-billion dollar settlements conclude years of litigation against pharmaceutical manufacturers, distributors and retailers filed by dozens of states and thousands of other plaintiffs. The complaints allege that the companies, like OxyContin maker Purdue Pharma, led a misleading, dangerous and ultimately deadly campaign to put pharmaceutical opioids into medicine cabinets across the country.
The agreements amount to some $50 billion nationally and more than $235 million for Maine. Two cases, Purdue and manufacturer Endo International, remain pending and could result in additional funds.
The coalition that issued the roadmap strongly warned against using the money on law enforcement, including “personnel, overtime or equipment,” or programs already funded.
The agreements say the funds must be used for “opioid abatement” and provide a hefty list of suggested strategies, but do not dictate whether the money should go to law enforcement beyond that.
But a Maine Monitor review of initial spending by the state, and some counties, cities and towns, shows a preference for existing programs, particularly those within or partnered with law enforcement agencies.
For example, Lewiston has spent more than $37,000 on a vehicle for Project Support You, a ridealong program started in 2018 that embeds a Tri-County Mental Health Services counselor with Lewiston and Auburn police and EMS departments. Additionally, it allocated $166,400 for city contracts with two Project Support You counselors in the current fiscal year’s budget, according to city administrator Heather Hunter and budget documents.
A $1,877 allocation to replace needle disposal boxes and $1,000 for the annual Rally for Recovery in this year’s budget pale in comparison.
Elsewhere, Sanford will spend more than $114,000 this fiscal year to “offset the cost of the police department’s mental health unit,” city manager Steve Buck told The Maine Monitor in late June.
Two full-time police officers, and one full-time and one part-time clinical social worker make up the mental health unit. “Future plans by the City Council will likely revolve around offsetting the cost of this successful program and associated treatment,” Buck said.
Sagadahoc County and the Brunswick Police Department plan to use some of the funds to hire a mental health liaison to work in both areas. The anticipated annual cost for Sagadahoc County is $37,000, county administrator Amber Jones said. Brunswick town manager John Eldridge said the police department is working out the details and no money has been allocated.
And in Westbrook, Chief of Police Sean Lally proposed using a portion of the city’s funds for the Westbrook Recovery Liaison Program.
“It represents a lack of imagination,” said social worker Charlotte Warren, a former state representative and Hallowell mayor.
“If we continue to do the same things we’ve always done, we will continue to get the same results we’ve always gotten. And that’s why I talk about this lack of imagination. We cannot let go of the idea that police should respond to drugs.”
In many communities, in Maine and nationally, mental or behavioral health clinicians are embedded within police departments to respond to crisis calls alongside law enforcement and to conduct follow-up visits with individuals. The Portland Police Department established the first co-response behavioral health unit in Maine in 1996 and today a number of departments statewide have similar programs.
For several decades, law enforcement agencies have been urged to use this community-oriented, “holistic approach” to mental health emergencies, especially because law enforcement are not specifically trained in mental and behavioral health, according to the U.S. Department of Justice.
This philosophy, however, has not been effective in achieving its goals, including improved community relationships and decreased interactions with law enforcement, according to advocates and the coalition that issued the roadmap.
Acknowledging that the settlement money has been “secured through the suffering of people who use drugs and their loved ones,” the coalition advised using it to “broadly address the damage of over 50 years of drug war policies grounded in criminalization, incarceration and anti-evidenced-based approaches to drug use.”
Zoe Brokos, the executive director of the Church of Safe Injection, said the roadmap and list of approved uses “made incredibly clear” that the settlement money should go to organizations and programming that work “directly with people at highest risk for opioid overdose.”
Jesse Harvey founded the Church of Safe Injection in 2018 as a mobile needle exchange-like program, handing out sterile supplies, fentanyl test strips and naloxone out of the back of his car. (Harvey died of an accidental overdose in 2020.) In 2021, CoSI became a Maine certified syringe service provider in Androscoggin, Cumberland and Oxford counties, and opened its first brick-and-mortar location on Main Street in Lewiston last year.
“We always try to have, like, an open and cordial relationship with law enforcement because it’s certainly easier than the alternative. But we do not work directly with them. We do not consider them community partners,” Brokos said.
“They have made that very clear that they don’t want to support the work that we’re doing.”
Lewiston Police chief David St. Pierre and public information officer, Lt. Derrick St. Laurent, did not respond to calls and emails requesting comment.
Amelia Smith, South Portland Police Department’s sole behavioral health liaison, said her presence has helped calm some people’s “super scared reactions” to seeing the police when she joins officers on a call.
Smith, a social worker, estimates she’s been on over 1,000 calls in nearly two years with the department. She averages two to three calls per day, in addition to follow-up calls where she meets people in the community or at their homes after a police interaction.
“I’m a really good buffer,” she said.
“I’m not in a uniform. (It’s) a breath of fresh air for them. They’re like, ‘Oh, OK, she’s not a cop.’”
South Portland appropriated about $104,000 in settlement money in this year’s budget to turn Smith’s position to full-time, and to hire an additional part-time behavioral health liaison, city manager Scott Morelli said.
While Brokos said CoSI has good relationships with the Project Support You counselors and OPTIONS (Overdose Prevention Through Intensive Outreach Naloxone and Safety) liaisons — a state-led program where behavioral health clinicians oftentimes work with public safety agencies — she would like to have seen the money go elsewhere.
In fact, the coalition’s “roadmap” specifically calls out the OPTIONS program as an example of “problematic spending” for working with police departments.
The Office of the Attorney General has allocated some of its settlement funds for OPTIONS, spokesperson Danna Hayes confirmed, in addition to $3 million for other substance use disorder programs within the Department of Health and Human Services.
Even with the “best of intentions,” some people may feel discouraged from using programs like OPTIONS simply because they often work alongside law enforcement, said Whitney Parrish-Perry, operating director for Maine Access Points.
Maine Access Points is a Maine CDC-certified syringe service provider serving all 16 Maine counties, with a focus on rural Mainers. It was one of the Maine signatories on the “roadmap” with Maine Recovery Advocacy Project and the Maine People’s Alliance.
“We hear all the time that folks don’t feel comfortable necessarily interacting with those folks, even if they are not employees of law enforcement entities,” Parrish-Perry said.
“And so my concern lies in a place where it feels like we have been here, this is what we’re already doing. And the settlement funds really call for innovative strategies through groups like Maine Access Points, providing on-the-ground peer support, providing the type of healthcare folks need as an entry point to get the other support and services they need,” she said.
Gordon Smith, Maine’s director of opioid response, said the coalition’s categorization of the OPTIONS program was “unfair” and based on a “significant misunderstanding” of how the liaisons work.
There are 16 OPTIONS liaisons — one for each county — and soon to be 16 more. They are hired and supervised by behavioral health organizations, like Sweetser, and may work alongside law enforcement but do not work for them, Smith said.
The OPTIONS model is most focused on connecting people to services after an overdose.
“The whole goal is everyone to work as a team to try to help people who are, you know, really struggling,” Smith said.
Besides OPTIONS, Smith pointed to Maine’s recently updated strategic plan for opioid response for examples of where settlement money would be well spent, which has “all kinds of innovative things.”
Even the priorities in the plan that are not new approaches nor particularly innovative, such as additional treatment and detox beds are “badly needed,” Smith said.
On that, advocates agree. Ryan Paige, an organizer with Maine Recovery Advocacy Project, and co-founder and chief operating officer of a nonprofit called AccessDirect Recovery Network, said the money should go to treatment and recovery programs where it can directly impact the people affected by the opioid crisis.
It should not be spent on programs “already being paid for by tax dollars,” like police department budgets, he said.
Paige, a Biddeford native who is in long-term recovery, said, for example, he often works closely with Maegan Lambert-Irish, the Biddeford and Saco police departments’ opioid outreach coordinator, and knows that “two truths can exist in the same space here.”
“One, she does wonderful work and she’s a wonderful person. Two, I still don’t think that the police department should be getting the money for these programs.”