At the Leonardville Nursing Home, a modest one-story building set back on a two-lane road on the edge of a small rural Kansas town of Leonardville (population 430 and dropping), Heather Germann worries day in and day out.
How is she going to get staff and keep them? She raised wages just recently, and that helped. But not enough. This year, lack of staff has meant that this 55-year-old nonprofit home cut back its population by 10 from the previous year, and fewer residents mean less income for the home.
Driving Germann’s worry is a proposed government rule that will require the nation’s nursing home to have a registered nurse (RN) on duty 24 hours a day, seven days a week, and establish minimum care hours per resident from registered nurses and certified nursing assistants (CNA).
The proposed rule, by the Centers for Medicare & Medicaid Services (CMS), was announced by the Biden administration in September, the first-ever minimum standards proposed at the federal level.
“It will force us to close,” says Germann, who has used her voice as the home’s administrator to lobby Kansas and federal officials about the dangers of the proposal.
But Missy Zirups, a licensed practical nurse (LPN) at the Good Samaritan Society in International Falls, one of only two skilled nursing facilities for miles in a far northern stretch of rural Minnesota, has a different concern. Will there be enough staff tonight and tomorrow to help her and others take care of residents?
When there’s one instead of two nurse aides on her shift, which is often the case, patient care is not what it should be, Zirups says. “Things are getting missed. People may not get their exercise or go for a walk or just get their personal time,” she says. “Medications can be late or missed or not ordered.”
She is sympathetic to pleas from her home’s administrators that they can’t find staff, but impatient with the burdens that means for her, her colleagues and the residents. The nursing home has a one-star rating, the lowest out of five, which is considered “much below average,” government reports show.
“Our International Falls location is well-positioned to provide the best care and support to our residents, and we staff to meet residents’ needs,” says an official in an email from the Good Samaritan Society, which operates the rural Minnesota home.
It is one of Good Samaritan’s 106 nursing homes, making it the nation’s largest nonprofit nursing home provider. (In 2019, the Good Samaritan Society merged with Sanford Health, the nation’s largest rural health care system).
These voices of nursing home workers and officials are part of a howling and sometimes fierce debate about the government proposal. It’s a debate that has been a long time coming, and which may offer a rare chance to realign care at the nation’s nursing homes, experts say.
On the one hand, the nursing home industry has grimly projected the eviction of thousands of elderly as a result of nursing homes closing or shrinking because of the rule.
Almost unanimous opposition to the rule comes from for-profit nursing home owners and operators, who account for about 70% of the nation’s estimated 15,500 nursing homes. Surprisingly, opposition to the rule also has the support of nursing home advocates such as LeadingAge, which represents nonprofit homes.
The proposal’s supporters respond that it’s time to improve care and they point to numerous studies showing that better staffing saves lives, improves residents’ physical and mental health and reduces needless avoidable medical and other costs.
“Honestly, why is it taking the country so long to do the right thing, both by residents and staff?” says Brenda Gallant, Maine’s long-term care ombudsman, who advocates for nursing home residents and their families, according to The Maine Monitor.
Indeed, supporters note that nursing homes in Alaska and Maine — two largely rural states with limited workforces — are the two top states where homes come close to meeting the proposal’s standards.
Nationally, only 1.1% of nursing homes met the proposed minimum care hours from both RNs and CNAs during the second quarter of 2023 (April to June), according to analysis from Barn Raiser, USA Today and Big Local News at Stanford University of the latest federal staffing data in the Payroll-Based Journal from CMS.
On average, nursing homes met the minimum care hours an average of 18 out of 91 days in the quarter. Nearly 40% of nursing homes across the nation did not have a single day in all 91 days of the quarter when they met the minimum staffing standards.
The state of rural nursing homes raises critical and compelling issues for the estimated 60 million rural Americans and the estimated 5,100 nursing homes that serve them.
Residents in rural nursing homes tend to be older and poorer and often face medical problems due to lack of medical care or access to hospitals and medical specialists. They have higher rates of dementia and mental health problems than the elderly in urban nursing homes.
And they often have to travel long distances to the nearest nursing home or even access emergency care, which can become a problem in sparsely populated areas. (Nursing home residents include more than people who are elderly. They also include people who are disabled or who need short-term medical support to recover after surgery or a health crisis, like a stroke).
A telling measure of rural America’s ill-health came with Covid-19.
Covid-19 hit rural America harder than many of the nation’s metro areas. By August 2022, the mortality rate among rural counties exceeded the rate for urban counties by 34%, with the highest death rates during those years in rural counties with higher percentages of Black and Hispanic residents.
On top of these challenges, rural communities also face the winnowing of nursing homes.
In 2018, over 1 million people lived in one of the 200 rural counties without a nursing home, according to a 2021 study by the Center for Rural Health Policy Analysis at the University of Iowa.
The study also found that, compared to urban areas, these closed rural facilities tended to have fewer beds, lower occupancy rates and were often linked to a local hospital.
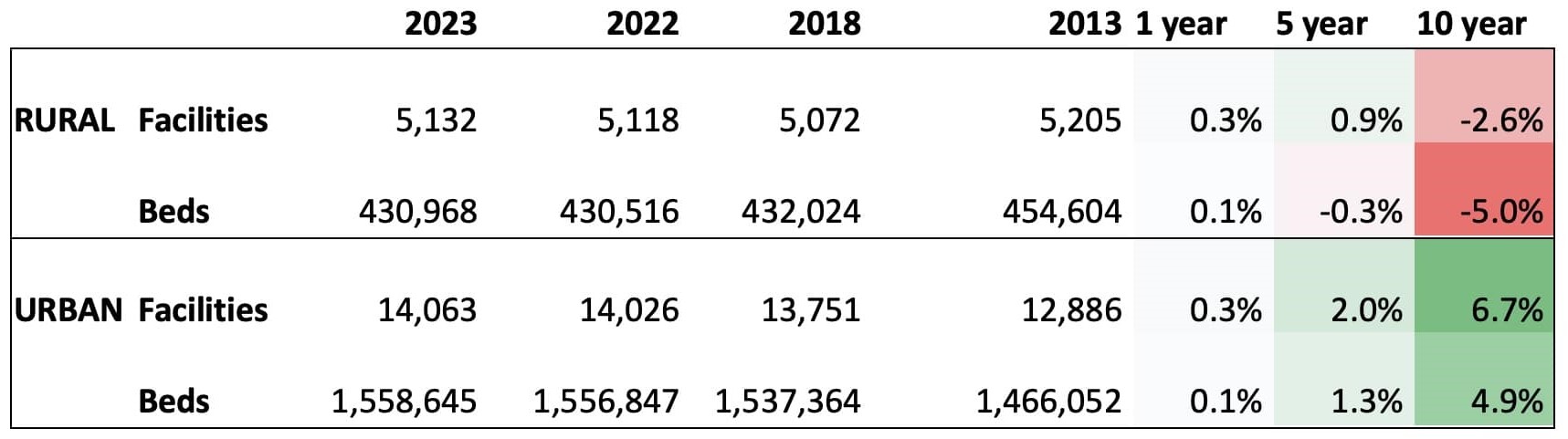
The number of nursing homes in rural areas is down 3% compared to 10 years ago but up slightly from five years ago, according to federal data from CMS. That stands in contrast to urban areas, where the number of facilities has increased 7% over the last decade.
Many of the problems intrinsic to rural communities today also impact the trend in nursing home closures. Nursing homes are often the largest employer around and usually staffed by local folks, which creates a comfort and familiarity that binds people in rural communities to their nursing homes. When a rural nursing home closes, the health care workforce in these communities shrinks.
What put the proposal on the government’s agenda now?
In February 2022, President Biden says the government would provide new rules to address the inadequate care provided at nursing homes across the nation.
Pointing to the 200,000 deaths that took place at nursing homes during the Covid-19 crisis, the White House says, “The pandemic has highlighted the tragic impact of substandard conditions at nursing homes, which are home to many of our most at-risk community members.”
Until now the government has only stipulated that nursing homes must have “sufficient” staffing to meet resident needs. And so, Biden’s proposed rule, which eventually emerged via an executive order in September, brought a minor earthquake.
The rule states that RNs must spend 0.55 hours daily with each resident, meaning a ratio of about one nurse for 44 residents. CNAs must devote 2.45 hours per day with residents, a ratio of about one CNA for every 10 residents.
At the same time, the administration says it would spend $75 million on training and scholarships for nursing home staff.
The proposed rule would give most nursing homes three years to meet the new standard, while rural nursing homes would have five years, with possible hardship exemptions available for facilities to maintain their Medicaid or Medicare license even if they do not meet the requirements.
While the rule was new for the federal government, 38 states and the District of Columbia have already set their own requirements.
But there are great discrepancies between states on how well their current requirements meet the government’s proposed standards.
One scholarly study released in November showed that just 1% of the homes in Louisiana would meet the hourly rules for RNs and CNAs; 4% in Texas, 5% in Arizona and 7% of the homes in Oklahoma and in Tennessee.
And though the staffing statistics for rural homes are similar to those in urban America, that does not take the pain or frustration away.
Consider Danielle Nickchen, who worked as a CNA for six years at various nursing homes in Wisconsin’s Door County, a rural Lake Michigan peninsula with a tourism-based economy. Inspired by the treatment given by nursing home staff for her adult daughter who died several years before, Nickchen wanted to offer the same level of care to others that her daughter received.
In 2022, burned out and saddened by her experience, she finally quit.
Taking care of people, the way they deserved was impossible, she recently told the Door County Knock. No matter how fast she moved to get residents ready, she could not get everyone down to breakfast on time.
The home where she worked between 2018 and 2022 — Scandia Village in Sister Bay, Wisconsin (also run by Good Samaritan Society) — has a one-star rating, according to government records, with a staff turnover rate of 83%. The national average is 52%.
A similar frustration haunts one CNA in central Pennsylvania.
“We give the best care we can in the condition that they staff us,” says a worker at the Northern Dauphin Nursing and Rehabilitation facility in Millersburg, who asked not to be named. “Back when I was first a CNA in ’96, we were allowed to have 12 aides on the day shift when we had 190 residents. … Now our census is 135 and we have six aides,” she says.
When there are not enough staff to deal with more needy patients, such as those suffering from dementia, “you have more falls,” she says.
The home is owned by Priority Healthcare Group, which has 18 facilities in Pennsylvania. The home has a one-star rating, as do 12 others owned by the firm in the state, according to government figures. The turnover rate for registered nurses at the Millersburg home, government reports show, is 72%.
Neither officials at the home, nor the company’s headquarters could be reached for comment despite repeated attempts over several days.

Adam Sholar, CEO of the North Carolina Health Care Facilities Association, says in an email that staffing problems doesn’t necessarily mean residents suffer. To deal with understaffing, facilities hire temporary agency workers, ask current staff to work overtime or limit their census, Sholar wrote.
Yet even with these measures, many North Carolina nursing homes will face problems meeting the proposed rule.
Among the 405 nursing homes across North Carolina, only 9 would have met the proposed requirement for hours spent by RNs with patients during the 91-day period in the second quarter of 2023, according to analysis from Carolina Public Press, USA Today and Big Local News. (Temporary agency workers and staff on overtime were included in the data, which also reflects the updated resident census at each facility.)
Rural nursing homes face a staffing conundrum
Understaffing often increases the risk of falls and other serious issues, while research shows that adequate staffing leads to better care, such as for dementia residents who benefit from having consistency in caregivers and daily routines.
Yet only so much can be done to overcome the staffing shortage says Rodney Rueter, President/CEO of Lutheran Sunset Ministries, which operates the Sunset Home in Clifton, Texas.
“We’ve been making it so far, but I don’t know much longer we can do this,” he says, adding that the home — the biggest employer locally in a town of about 3,400 — has been thinking about finding a partner that can run the home “more efficiently.”
“When a nurse’s aide pay is close to the pay at fast food operation, it’s hard to find workers,” Rueter says. And it’s especially hard in Texas, he says, since the state has long been at the bottom among the states in terms of Medicaid reimbursements.
While the federal government sets rates for Medicare, which covers up to 100 days of a short-term stay for people who qualify, states set the rates for Medicaid, which covers long-term stays in nursing homes, and is partially reimbursed from federal dollars.
Even though Sunset Home has a four-star rating by the government, it doesn’t match up to other homes on the time nurses spend with patients. That’s clear once you understand its lack of nurses.
Sunset Home currently does not have any RNs on night shift during the week, the weekend RN works double shifts covering afternoons and night shifts, and there’s no day shift RN on Saturdays and Sundays. Saying that the home is already in “financial straits,” Rueter estimates that it would cost $1 million to add the staff needed under the government proposal.
Backing up Rueter’s complaint about the difficulty of adjusting to the new proposal, the National Rural Health Association (NRHA) has told the government that it should either withdraw the minimum staffing standard or at best exempt rural facilities. Poor outcomes cannot be solved by setting staffing minimums, it said.
The solution, the NRHA suggested, is boosting the number of nurses.
“We want to emphasize that we are concerned with quality just as the CMS (Centers for Medicare and Medicaid Services) are … but we don’t believe in imposing one-size-fits-all nursing homes,” says Alexa McKinley, regulatory affairs manager for the NRHA in an interview.
Good, but not good enough
The blunt reply from nursing home advocacy groups and union health care workers to all of the handwringing from the nursing home industry is that the proposed rules are good, but not good enough.
Advocacy groups say the government could have chosen higher staffing standards that have been recommended since a 2001 study by CMS, and they are wary of exemptions in the proposal that could offer loopholes to companies without improving care.
Mark C. Miller, president of the National Association of State Ombudsman Programs (NASOP) and a long-term ombudsman for the District of Columbia, said his group supports the proposal. But it is against the five-year exemption for rural homes, arguing that taxpaying rural elderly should not wait to get quality care. Instead, the group says that the rule should be phased in over two years.
The NASOP also argues that the homes that receive exemptions should not be allowed to add new residents until they met the new requirements. They also say that exemptions should not be granted to nursing homes with histories of poor care of their residents.
Lori Smetanka, executive director of the National Consumer Voice for Quality Long-Term Care, goes a step further. She thinks nursing homes should not be able to endlessly renew their exemptions. “We need to ensure that residents get the care they need,” Smetanka says.
For some, however, the battle is not simply fixing the proposal but getting it to become reality as the political wrangling gets under way.
“The nursing home industry is very powerful, and they have a lot of money,” says Lee Goldberg, an official with the AFL-CIO who has guided the labor federation’s support for the staffing proposal.
Like others, Goldberg suspects that the industry doesn’t disclose its true finances, and hopes that a proposed rule on transparency for the industry will clear up some concerns. “They [the nursing home industry] are willing to lie through their teeth and scare people,” he adds.

In its explanation for the transparency rule, the Biden administration noted a surge in facilities changing ownership, with 3,000 nursing homes having changed hands between 2016 and 2021.
Many of these were one-star facilities, raising questions about whether the new owners had improved the homes’ quality.
Nonetheless, believers in stronger federal oversight of the nursing home industry feel that the facts are on their side.
And they have been buoyed by award winning USA Today investigations that have found nursing homes are rarely punished for breaking rules, and penalties remained sparse even when inspectors found low staffing had factored into incidents of deaths, broken bones and negligence.
The rule’s uncertain future
How will the rule play out?
Several years at least of haggling and amending it, if it survives, experts say. Yet even a watered-down rule will make a difference, experts add, because the worst homes will be targeted and cut out.
For starters, it’s likely that the government will need a year to go through the more than 46,000 comments that poured into the public register on the rule. So, far a group of Republican governors have weighed in, voicing their disapproval of the proposal and House Republicans have been outspoken in their opposition.
U.S. Sen. Deb Fischer (R-Neb.) has recently led the charge against the proposal, introducing a bill that would block the government from enacting the proposal on the account that it would hurt rural homes in her state and force some to close.
Meanwhile, the issue has divided some Democrats. In November, U.S. Sens. Elizabeth Warren (D-Mass.), Bernie Sanders (I-Vt.), and Richard Blumenthal (D-Conn.) issued a detailed report in favor of the proposed rules, and Sen. Bob Casey (D-Penn.) has used his influential role as Chairman of the U.S. Senate Special Committee on Aging to support Biden’s proposal.
However, a recent bipartisan letter by Sen. Jon Tester (D-Mont.) argued against the proposal. Tester was joined by other Democratic lawmakers, many from rural districts, along with more than 20 Republicans.
A leader in the resistance to the rule is the American Health Care Association (AHCA), which represents both for-profit and nonprofit nursing homes. The AHCA has steadily aired its disapproval of the rule, and will likely exercise its political powers in Washington.
A well-financed voice for nursing homes and other health care organizations, it spent $3.99 million in lobbying in 2022 — its second highest sum in recent years — and just over $1 million in campaign contributions, according to Open Secrets, an organization that tracks political funding.
“The proposed staffing rule is an overreaction — a poor reaction to a horrible crisis that we all experienced,” said Mark Parkinson, the CEO and president of the AHCA.
A former governor of Kansas and former owner of nursing homes in Kansas and Missouri, Parkinson was speaking at an organization meeting in October, where he reminded the audience about the health care industry’s ability to overturn policies it considers unfavorable.
However, Alexa McKinley of the National Rural Health Association, expects the rule to take effect in a form similar to its original but with some tweaks, she says in an interview.
As for fixing nursing homes, CNA Viometrice Simmons is a hands-on expert, who knows what needs to be fixed and how to do it.
The bulk of hands-on work in nursing homes is done by CNAs like Simmons. They are 91% female, more than half are minorities and one out of five are immigrants. Their median wage in 2022 was $17.06 an hour, meaning they earn less than a living wage in most communities. And they suffer on the job injuries more than eight times the rate of other workers.
In 30 years of working as a nurse’s aide in Mississippi, Simmons, who is 52-years-old, has earned her experience with grit and sweat and for menial wages. She earns $17 an hour today after all her years of experience. Another home recently tried to lure her away, but they were only paying $15 an hour.
Here’s one of her solutions: “When you walk in that door every resident is your patient,” she tells Mississippi Today.
“I’ve seen patients asking to go to the bathroom over and over and the staff is running around, [saying] ‘Let me see who got you’ and ‘You got a diaper and go in the diaper.’ No that’s unacceptable. If someone has to go to the bathroom, I don’t care who it is, if you are able to take that person to the bathroom, you are supposed to get up and taken them to the bathroom.”