In the years before the COVID-19 pandemic swept through the nation’s long-term care facilities and overwhelmed healthcare workers, Maine nursing homes increasingly hired nurses and nursing assistants through outside agencies to prevent staffing shortages.
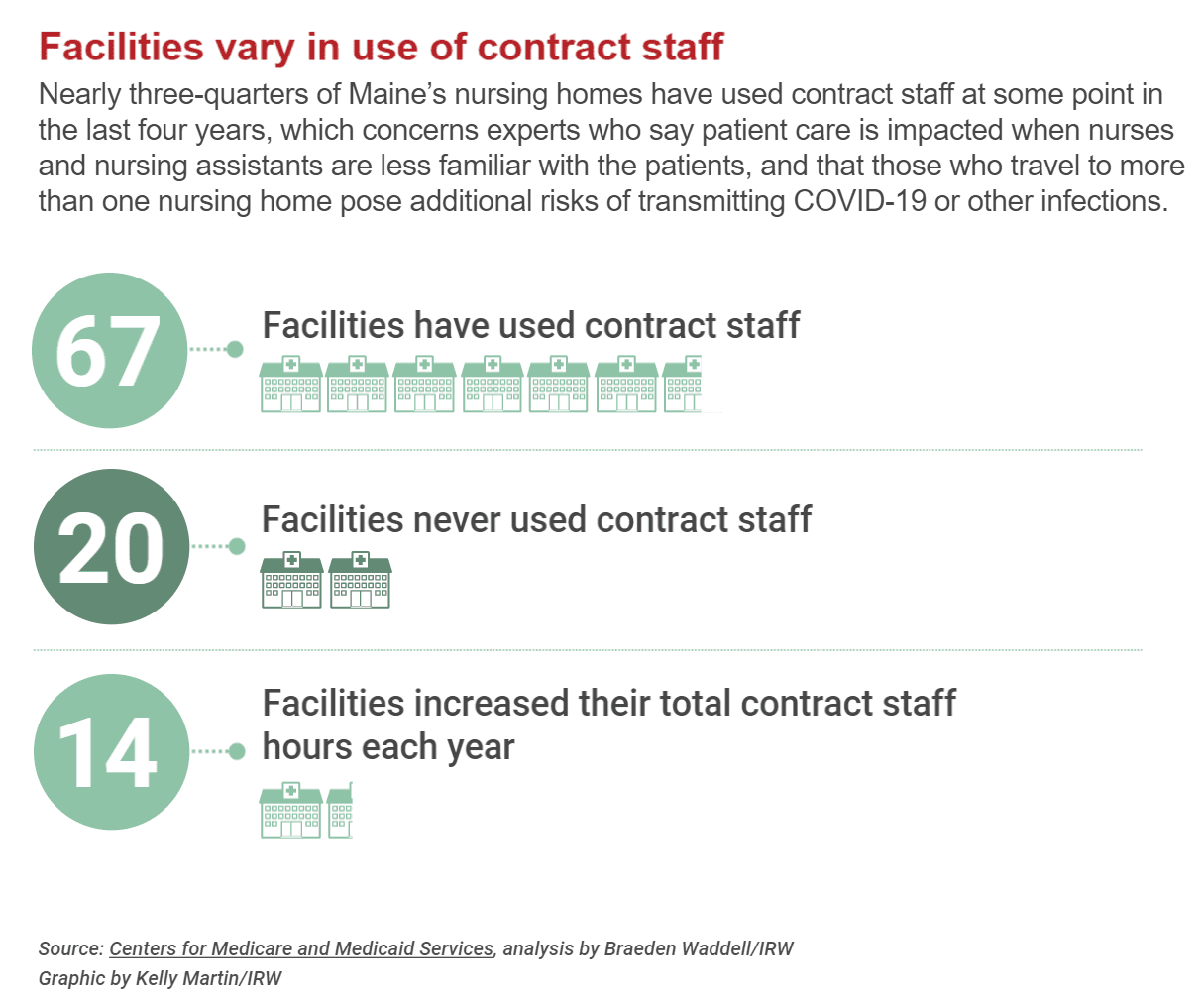
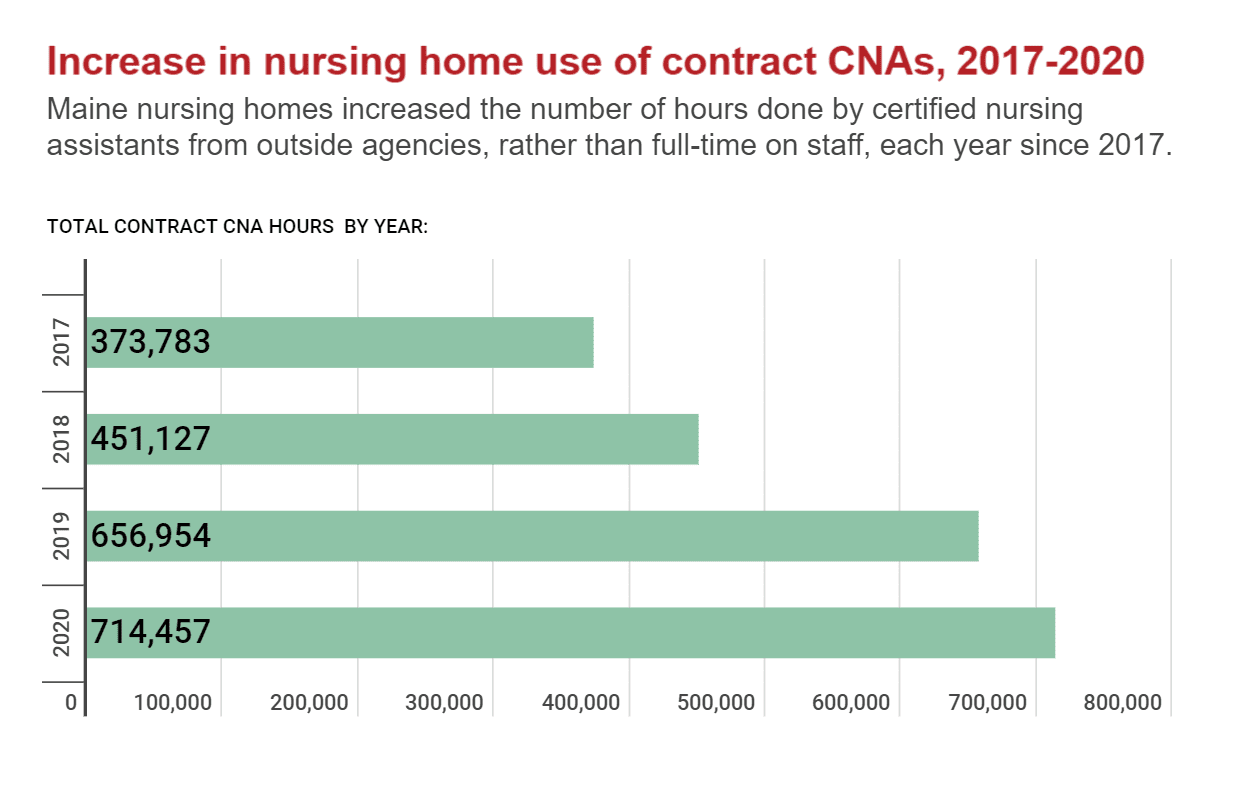
A four-month investigation by The Maine Monitor and Investigative Reporting Workshop found that contracted hours for certified nursing assistants in nursing homes across the state have nearly doubled since 2017. And agency staffing hours across all employee types rose 66% during that same period.
These contracted traveling nurses and nursing assistants, initially intended as a stopgap during an emergency or staff shortage, are increasingly becoming the norm, according to federal data and more than a dozen interviews with nursing home administrators, educators, staffing agencies and state officials.
The investigation did not find a direct relationship between higher rates of contracted staff in Maine’s 93 nursing homes, and COVID-19 cases and deaths at those facilities. But experts still raised concerns about the trend, highlighted by and expanded during the pandemic.
The challenges are expected to grow as Maine’s population ages and pandemic burnout pushes healthcare workers out of the industry.
While some experts say contract staffing is a necessary but expensive tool to meet mandatory staffing ratios during a crisis, the increasing reliance on short-term agency staff raises concerns about quality of care.
At least one study prior to the pandemic linked high use of contracted staff to negative health outcomes for residents. And as COVID-19 reached congregate living settings, experts worried that workers moving between facilities could cause outbreaks.
But nursing homes that use these agency workers argue that they don’t get enough qualified applicants to fill permanent positions, which historically have been undervalued, underpaid and largely female.
In addition, this reliance on contracted staff — rather than on full-time health workers who know their patients’ needs and can spot changes — can differ dramatically among nursing homes. While most facilities used contracted workers, 20 have not done so for the last four years. And five homes used such workers for more than half of their CNA direct-care hours in 2020.
Maine nursing homes have reported that agencies are rapidly accelerating their rates for contracted staff during the pandemic, said Rick Erb, former president and CEO of the Maine Health Care Association, which represents 200 nursing homes and assisted living facilities.
“There’s sort of an arms race here going on,” Erb said. “I believe that we would have seen this trend at a slower rate (but) the pandemic has accelerated it.”
St. Mary’s D’Youville Pavilion in Lewiston used contracted CNAs for about 35% of its direct-care hours performed by CNAs last year. Administrators said they increased their rates and offered hiring bonuses to attract permanent employees, but competition is steep for the few qualified candidates, and their paid CNA training program often has open seats.
Some experts said nursing homes view contracted hours as a “black mark.” Reporters reached out to nearly 40 nursing homes that used agency staff in recent years and heard back from only a handful. But Brenda Laplante, director of employee experience for the St. Mary’s Health System, pushed back on that description.
“Obviously, the cost is a factor, but we don’t think of it as a black mark at all,” she said. “We will do what we need to do to make sure we have the highest standards of patient care.”
Trapped in a ‘vicious cycle’
The reliance on contracted nurses and CNAs has ebbed and flowed over the past two decades, often in tandem with the economy, said Erb, who served as president and CEO of the Maine Health Care Association for 20 years until retiring at the end of June.
Contract nurses and CNAs are valuable as a “just in time” solution to sudden staff shortages, Erb said. But in recent years, facilities have used them more and more, not only in emergencies.
“What becomes more ominous is when you become overly dependent on staffing agencies,” Erb said. “That’s not somewhere that any facility wants to be.”
Experts worry that residents will suffer the consequences of more staff turnover and possible gaps in training associated with contracted staff.

Permanent CNAs gain an “intuitive sense” of what their residents need and when their conditions worsen, said Stephen Campbell, a data and policy analyst at nonprofit PHI, which advocates for direct-care workers. Contracted staff don’t have a chance to build those relationships.
And facilities that rely heavily on contract staff may find it difficult to replace those workers with direct employees in the future.
“In some ways, it becomes this vicious cycle of expending more resources to bring in staff, taking away from resources that could be spent on recruitment, retention efforts,” Campbell said.
A reduced reliance on agency staff in Maine nursing homes in the years before the pandemic likely would have prevented some COVID-19 outbreaks, Campbell said. Contracted staff moving between facilities during a pandemic presented “an additional danger at a time when working conditions were already extremely dangerous.”
During the pandemic, the Maine Health Care Association told its member nursing homes to avoid moving workers from one facility to another as much as possible. Erb said he was concerned about contracted employees transmitting COVID-19 among facilities but wasn’t certain it was a “key factor.”
The larger problem was the asymptomatic nature of COVID-19 and the difficulties of detecting it among staff, he said, especially in the early days of the pandemic before testing was widespread.
About 70% of Maine nursing home staff are now vaccinated against COVID-19, according to the state Department of Health and Human Services, the ninth-highest rate in the country. Still, that means for every 10 nursing home workers who deal with patients, three are unvaccinated, and can still get and transmit the virus.
Patients with bedsores, depression
Facilities with more than 25% agency staff had higher percentages of residents with a number of health issues, including high levels of anxiety and depression, more bedsores and decreased mobility, according to a 2009 study conducted by Nicholas Castle, a national expert on patient-care and staffing ratios, and now department chair of Health Policy, Management and Leadership at West Virginia University’s School of Public Health.
In a recent interview, Castle said too much reliance on temporary staff is a red flag indicating other problems within the facility related to poor administration, management or long-term planning.
Castle said any facility with more than 10% of its total hours done by contract staff faces a precarious situation. Facilities with more than 25% were the “worst of the worst” when it comes to quality issues for residents.
“Would I put my parents in a nursing home that is hiring high amounts of agency staff? Absolutely not,” Castle said. “If my parents were in a facility that started hiring more and more agency staff, I would be, let’s say, vigilant.”
Maine nursing homes, however, have a high bar to meet for standards of care. The state’s minimum staffing ratios are among the highest in the country, said Brenda Gallant, the state’s long-term care ombudsman. The ombudsman program is an independent nonprofit that advocates for residents and investigates complaints on their behalf.
Nursing homes are required by state law to have one direct-care staff member for every five residents during the day; one for every 10 residents in the evenings; and one for every 15 residents overnight. As a result of those ratios, Maine historically has had fewer deficiencies of care, Gallant said.
It’s crucial to have enough staff who can help residents with activities such as dressing, bathing and eating, Gallant said. But it’s also important that these caregivers know the residents and can recognize small changes.
“A resident with dementia may not necessarily be able to tell somebody that they’re not feeling well,” Gallant said. “But a staff person who knows them might see a change in their behavior that is more subtle and pick up on it.”
Rising demand, shrinking workforce
As the U.S. population ages and current healthcare workers retire, there aren’t enough young professionals filling the gaps.
A study of physician shortages from the Association of American Medical Colleges found that the U.S. population under 18 is projected to grow about 4% by 2033, whereas the population 65 and older is projected to grow 45%.
That problem is especially pronounced in Maine, which not only has the oldest median population in the U.S. but also a dwindling youth population.
By 2040, there will be only two working-age Mainers for every adult over 65, according to a March 2020 study by the University of Southern Maine. In 2000, that ratio was 4.1 working Mainers for each person over 65.
Registered CNAs in Maine increased 15% between January 2015 and January 2020, according to the state Department of Health and Human Services.
However, Maine is projected to have a total nurse shortfall of 2,700 by 2025, said Kelley Strout, associate professor and director of the University of Maine School of Nursing.
She cited a lack of faculty and clinical training sites that forces nursing schools to turn away qualified applicants.
And filling shortages in long-term care is more difficult than others because those positions are physically and mentally demanding, Strout said. Nursing students overwhelmingly say they want to work in a hospital.
“You very rarely hear students say their dream career in nursing would be in a specialty such as long-term care, or caring for older adults, or working in a jail, or even working in primary care,” Strout said. “I really think it has a lot to do with media and imaging that we see our whole lives.”
Coupled with the students’ views of working with the elderly is the relatively low pay. The statewide average hourly wage for nursing home CNAs — 90% of whom are female — is about $16, but it varies based on geography and the size of the facility, according to the Maine Health Care Association. Registered nurses, who have more training, average about $31 an hour.
Nursing home wages are low in part because 70% of residents are covered by MaineCare, said Erb, with the Maine Health Care Association. That means nursing homes have tight profit margins, which makes it difficult to raise salaries.
The average CNA wage increased 10% between spring 2020 and spring 2021, which speaks to the demand, Erb said. While they appreciate the increases, “the need is outpacing the support.”
To address the growing need, the state Department of Health and Human Services has launched an online tool for facilities to connect with qualified applicants; worked with staffing agencies to ensure costs are transparent and consistent; collaborated with the university and community college systems to enhance their nursing programs; and expanded CNA training programs and guided facilities developing their own programs, said spokeswoman Jackie Farwell.
New legislation will increase reimbursement rates for direct-care workers to 125% of the minimum wage and tie future increases to increases in the minimum wage.
These wages have stagnated for years while businesses such as McDonald’s and Walgreens have increased their pay, said Jessica Maurer, executive director of the Maine Council on Aging, a coalition of industry representatives and aging advocates. Some workers switch industries because there isn’t an incentive to continue the often highly physically and psychologically demanding responsibilities that come with working in a nursing home.
And in Maine, that’s only part of the problem.
Maurer added that Maine nursing homes in rural locations rely heavily on recruiting new workers directly from their communities. But if they can’t find employees locally, they need to hire contract staff for extended periods to ensure they are meeting the ratio of CNAs to residents required by the state.
“Nursing homes are in violation of staffing ratios the second somebody doesn’t show up to work,” she said, “and so they have to maintain their staffing and they have to hire agency staff, which is a much higher cost.”
‘A role born out of crisis’
While the pandemic brought attention to staffing problems in long-term care, the change in contracted hours in Maine from 2019 to 2020 was actually the lowest increase in contract staff hours in the last four years.
Three national staffing agencies told reporters they also have noticed an uptick in demand for their nurses in recent years, and they seem to have conflicting thoughts about what that means for the industry as a whole.
The pandemic amplified the need for traveling nurses and CNAs, but the demand had grown for at least 20 years, according to representatives of Medical Solutions, which provides traveling nurses to about 2,200 facilities across all 50 states.
Traveling nurses received more attention recently for deploying to COVID-19 hotspots, particularly in long-term care in which the population was more vulnerable, said Todd Davis, director of operations with Medical Solutions, a national staffing agency headquartered in Nebraska. And they were crucial in facilities that had permanent staff who were sick themselves during the height of the pandemic.
“If (nursing homes) could staff it all themselves, absolutely they should and I’m OK with that,” Davis said. “The problem with the state of the market and things now is the demand is there because most facilities don’t have those capabilities.”
Agencies such as Medical Solutions recruit and vet the traveling nurses and CNAs. Often included in their flat rate are costs related to certifications and benefits, such as retirement matching, health insurance, malpractice insurance and payroll tax. The agency workers also may receive a tax-free per diem for lodging and a per diem for meals.
During the pandemic, rates for traveling nurses shot up to sometimes threefold what a nurse or CNA would make at a permanent position.
But “there’s a lot of sacrifice,” said Michael Elm, senior business development manager for staffing firm All Medical Personnel. “They’re there to fulfill a specific role and that is a role that was really born out of crisis.”
They have to travel around the country and learn new facilities. The typical stint is 13 weeks but can sometimes grow to a year. Some nurses become permanent staff after their three-month stint, but for many the flexibility and temporary nature of the job is what appeals to them, Elm said.
He said travel nurses and CNAs are highly skilled and often have years of experience. He argued that there’s less turnover because they are at a facility for a shorter period and therefore have more endurance. And they can bring an outsider’s perspective on what might not be working in a facility.
But he conceded that there is value in having a permanent team dedicated to the long-term success of the organization. “Travel nursing can’t necessarily give you that,” he said.
A way forward
Nearly one-quarter of Maine nursing homes never used contracted staff between 2017 and 2020. Some administrators said hiring agency staff was a slippery slope — a slope the pandemic nearly pushed them down.

Durgin Pines in Kittery reported zero contract hours for any direct-care workers since 2017. Lauren Scogin, the administrator, said Durgin Pines has worked to avoid contract staff in the past. But that changed when the facility faced its second COVID-19 outbreak and had to hire a contracted nurse for a few weeks in November.
Even when she turned to temporary staff, it was difficult to hire someone.
“We had about three different staffing contracts because we really just needed to get somebody in the building,” Scogin said. “It took a while to get a nurse, so it’s not a quick, easy fix. It’s not guaranteed.”
Dr. Jabbar Fazeli, who serves as medical director at Durgin Pines and another Maine nursing home, said the best way to avoid needing contract staff is to take the money spent on outside employees and invest instead in training, recruitment and retention.
“But that’s easier said than done. Obviously, if you ask any of them, they will tell you they’re trying,” said Fazeli, a prominent geriatrician and vice president of the Maine Medical Directors Association.
It’s especially hard to retain CNAs because they often don’t get paid a living wage and their skills overlap with other jobs that could pay more, Fazeli said. Nurses have more professional training geared toward a specific career, he said, so they are less likely to leave the industry altogether.
Some facilities have CNA courses in which they train people they hope will stay with that nursing home. Genesis HealthCare, which operates 11 Maine nursing homes, said in a statement that it has hired CNA instructors for classes at two of its facilities: Marshwood Center in Lewiston and Oak Grove Center in Waterville.
“These classes are projected to significantly reduce Marshwood Center’s agency staffing over the next two months, and Oak Grove is projected to be agency-free by the end of the third quarter of 2021,” spokesperson Lori Mayer said.
Starting a facility training course can be “daunting,” Fazeli said, but pays off in the long run. As nursing homes train and recruit more employees, they can shift their incentives from new hires to rewarding the existing staff who have stuck around.
Fazeli emphasized, however, that rising agency hours in nursing homes is a systemic concern, not a negative reflection on individual agency workers. The contracted staff he worked with “were great professionals.”
“It’s just the consistency factor — getting used to a place and working with the same people over and over again, especially the residents who need you to know them before you can care for them properly,” Fazeli said.
In December, Caribou Rehab and Nursing had a devastating COVID-19 outbreak that infected all 59 residents and 30 of its 140 employees. The Maine CDC linked five deaths to the outbreak, but the administrator, Phil Cyr, estimated that COVID-19 contributed to another seven for a total of 12 resident deaths. After the outbreak, many of their direct-care employees walked away from the industry for good.
Cyr stopped accepting new residents for a few months to avoid hiring caregivers outside his full-time workforce. And he worked with students getting their certifications who could then become employees at the facility.
Caribou Rehab and Nursing never has used contracted staff in its 43 years, Cyr said. He partners with local adult education programs and allows them to use his facility for training to ensure there are enough CNAs coming up to fill his open positions.
Cyr said he hopes he’ll “never” need to hire contract staff because the added costs could lead to worse ratios and quality of care, which could devastate a facility’s reputation in the tight-knit communities of northern Maine.
“Everybody knows everybody. And so who you’re taking care of at the nursing home is your neighbor, your neighbor’s mother, or your mailman, his father,” Cyr said. “You have a personal reputation to take the best possible care of everybody in your building.”
The Investigative Reporting Workshop (IRW) is a nonprofit, independent newsroom based at American University.








